The Role of Neutrophil to Lymphocyte Ratio (NLR) and Platelet to Lymphocyte Ratio (PLR) in Appendicitis
on
DIRECTORY OF
OPEN ACCESS
JOURNALS

The Role of Neutrophil to Lymphocyte Ratio (NLR) and Platelet to Lymphocyte
Ratio (PLR) in Appendicitis
Moch Junaidy Heriyanto1, Tri Ratnaningsih2*, Rona Hafida Heriyanto Putri3, Bunga Fatimah2, Fardhiasih Dwi Astuti4
-
1 Department of Surgery, Universitas Ahmad Dahlan, Yogyakarta, Indonesia.
-
2 Department of Clinical Pathology, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia.
-
3 Faculty of Medicine, Universitas Ahmad Dahlan, Yogyakarta, Indonesia.
-
4 Department of Public Health, Universitas Ahmad Dahlan, Yogyakarta, Indonesia.
*Corresponding author: triratnaningsih@ugm.ac.id.
ABSTRACT
Aim: Predictive values of neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) are associated with poor outcomes in several diseases. Furthermore, there has been limited publication of those parameters in appendicitis patients in Indonesia. This study aims to evaluate the role of NLR and PLR in differentiating complicated appendicitis and uncomplicated appendicitis. Methods: The design of this study is a retrospective using medical records of appendicitis patients from January 1, 2016, to December 31, 2020, conducted at PKU Muhammadiyah Bantul Hospital. There are 408 data on appendicitis patients that can be analyzed. Results: The WBC, neutrophils, NLR, and PLR was significantly higher in the complicated appendicitis group than in the uncomplicated group [11,5 (3.79-35.2) vs. 8.42 (3.32-39.30), p<0.0001; 8.63 (2.359-2.647) vs. 5.446 (1.691-35.960), p<0.0001; 5.65 (0.95-23.86) vs.3.82 (0.81-23.86), p<0.0001; 168.57 (37.27-974.03) vs.139.40 (56.84-1274.31), p<0.0001, respectively] followed by a significantly lower lymphocyte count [1.709 (0.154-5.71) vs. 2.094 (0.401-5.812), p<0.0001, respectively]. The area under the receiver operating characteristic (ROC) curve, cutoff point, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio of NLR for diagnosis of complicated appendicitis were 0.76, >2.84, 75.21%, 62.65%, 74.6%, 63.4%, 2.01, 0.40, respectively. In contrast, an area under ROC curve, cutoff point, sensitivity, specificity, PPV, NPV, and likelihood ratio of PLR for differentiating complicated and uncomplicated appendicitis were 0.605, >140.6, 65.70%, 51.81%, 66.5%, 50.9%, 1.36, and 0.66 respectively. Conclusion: The cutoff values of NLR (>2.84) and PLR (>140.6) were significant diagnostic parameters for complicated appendicitis (p = 0.0001). Hence, NLR and PLR can assist in diagnosing complicated appendicitis.
Keywords: appendicitis, NLR, PLR.
DOI: https://doi.org/10.24843/JBN.2024.v08.i01.p01
INTRODUCTION
Acute appendicitis is the most common cause of acute abdominal pain. The incidence of acute appendicitis in Indonesia is estimated at 95 cases per 1000 population and ten million cases annually. Appendicitis cases in infants are relatively low. It increases in childhood, reaching a peak at 10-30 years old. Appendicitis occurs 1.3-1.6 times more
frequently in men.1 Acute appendicitis requires immediate action to prevent complications that can increase morbidity and mortality. The complications include perforation, abscess, intestinal obstruction, peritonitis, and sepsis. Diagnosing acute appendicitis remains challenging because its signs and symptoms often mimic other abdominal diseases.2 Thus, it is often missed.
As many as 30% of patients with proven appendicitis reported receiving other diagnoses previously and were discharged instead of being treated accordingly. Errors in diagnosing appendicitis are the fifth leading cause of successful litigation against physicians in the emergency department. They account for 15% of fines paid in malpractice claims in the emergency department.3
Several decades ago, under certain conditions, negative appendectomy (NA) was acceptable to prevent morbidity and mortality due to perforation.4 However, currently, NA is no longer acceptable. Researchers developed several clinical scoring systems for acute appendicitis to prevent NA and improve the accuracy of preoperative diagnoses, such as Alvarado, Eskelinen, Ohmann, AIR, RIPASA, Tzanakis, Lintula, Fenyo-Lindberg, and Karaman.5,6
Several studies report a high rate of perforation in appendicitis, which is 15-45%, while the NA rate is 7-25%. This rate shows that with the development of technology and clinical experience, the perfect method of diagnosing appendicitis has not yet been found.4 Imaging modalities, such as ultrasonography (USG) and computer tomography (CT-scan), are considered insufficient to diagnose properly despite their high cost and more sophisticated imaging capabilities.6 Other examinations, several hematological parameters, can diagnose acute appendicitis. This examination is available throughout the hospital, affordable, and relatively fast.
A leukogram, including leukocyte count and type count, helps diagnose appendicitis. Leukocytosis above 20,000 cells/mm3 may indicate a perforation and requires immediate action.7 An increase in the percentage of polymorphonuclear >85% is associated with the severity of diseases such as necrosis and perforation.8 The lymphocyte count in patients
with severe appendicitis is significantly lower than in the early stages.9 Recently, studies reported the predictive value of neutrophil to lymphocyte ratio (NLR) in inflammation, which can be used as a diagnostic parameter in the perioperative diagnosis of acute appendicitis. Apart from NLR, platelet-to-lymphocyte ratio (PLR) is also associated with poor outcomes in several diseases.10 Furthermore, publications on NLR and PLR in appendicitis patients in Indonesia are still limited. This study examines the role of NLR and PLR to distinguish complicated appendicitis and uncomplicated appendicitis.
METHODS
Patient Population
This diagnostic test study was a retrospective design using medical records of acute appendicitis patients. The subjects of this study included acute appendicitis patients at PKU Muhammadiyah Bantul Hospital who were diagnosed with acute appendicitis both clinically and anatomically from January 2016 - December 2020. The exclusion criteria were acute appendicitis patients with other inflammatory diseases or incomplete data on their medical records. The variables studied included data on the characteristics of subjects: clinical, laboratory, and imaging examination results. This research has obtained permission from the Faculty of Medicine, Public Health, and Nursing Universitas Gadjah Mada (FK-KMK UGM) ethics committee with ethical eligibility Number: KE/0067/01/2021.
NLR and PLR measurement
Neutrophil and lymphocyte counts were examined using a hematology analyzer. The NLR and the PLR were calculated as the ratio of neutrophil count to lymphocyte count and platelet count to lymphocyte count, respectively.
Statistical analysis
We checked the collected data for completeness, then coded, tabulated, and entered it into the computer. Subject characteristic data are presented descriptively in mean ± standard deviation if the data distribution is normal, or median (min-max) if the data distribution is not normal, and categorical data are present in frequency and proportion.
RESULTS
We acquired 429 patients data with acute appendicitis. There were 21 data excluded due to other inflammatory diseases or incomplete data. The variables studied included clinical
and laboratory data on the characteristics of subjects. Hematological parameters in the medical record were hemoglobin, leukocyte count, type count, and platelet count. Clinical parameters recorded were operative diagnosis: complicated appendicitis and uncomplicated appendicitis. We analyzed 408 subjects in this study, as shown in Table 1.
Parameters tested by Receiver Operating Characteristic (ROC) were the number of leukocytes, neutrophils, Neutrophil Lymphocyte Ratio (NLR), and Platelet Lymphocyte Ratio (PLR). The ROC test results are shown in Figure 1, Table 2, and Table 3.
Table 1. Comparison of sex, age, and hematological parameters in complicated and uncomplicated appendicitis group.
|
Variable |
Complicated appendicitis n=242 |
Uncomplicated appendicitis n=166 |
p |
|
Sex n= (%) | |||
|
Male |
158 (65.3%) |
55 (33.1%) |
0.0001a |
|
Female |
84 (34.7%) |
111 (66.9%) | |
|
Age (years old) |
33 (1-80) |
25 (2-95) |
0.025b |
|
Hemoglobin (g/dL) Mean (SD) |
13.62 (1.82) |
13.32 (1.48) |
0.08c |
|
Platelets count (x103/µL) |
278,5 (150-802) |
289 (165-758) |
0.136 b |
|
White blood cell count (x103/µL) |
11,5 (3.79-35.2) |
8.42 (3.32-39.30) |
0.0001b |
|
Neutrophil (x103/µL) |
8.63 (2.359-2.647) |
5.446 (1.691-35.960) |
0.0001b |
|
Lymphocyte (x103/µL) |
1.709 (0.154-5.71) |
2.094 (0.401-5.812) |
0.0001b |
|
Neutrophil-to-Lymphocyte Ratio (NLR) |
5.65 (0.95-23.86) |
3.82 (0.81-23.86) |
0.0001b |
|
Platelet-to-Lymphocyte Ratio (PLR) |
168.57 (37.27-974.03) |
139.40 (56.84-1274.31) |
0.0001b |
Note: Result showed in Median (Min-Max); a.Chi-square; b.Mann Whitney; c.Independent t-test, significant if p<0.05.
Table 2. The AUC value of Hematology parameters for diagnosing complicated appendicitis.
|
Parameter |
AUC |
IK 95% |
p |
|
WBC count |
0.697 |
0.646 – 0.748 |
0.0001 |
|
Neutrophil count |
0.721 |
0.671 – 0.771 |
0.0001 |
|
Neutrophil-to-Lymphocyte Ratio (NLR) |
0.726 |
0.677 – 0.775 |
0.0001 |
|
Platelet-to-Lymphocyte Ratio (PLR) |
0.605 |
0.550 – 0.659 |
0.0001 |
Note: AUC: Area Under the ROC Curve.
Table 3. Diagnostic ability of Hematology parameters for diagnosing complicated appendicitis.
|
Parameter |
COV |
Sn |
Sp |
+PV |
-PV |
LR (+) |
LR (-) |
YI |
|
WBC count |
>8700 |
73,55 |
56,02 |
70,9 |
59,2 |
1,67 |
0,47 |
0,33 |
|
Neutrophil count |
>6127 |
72,31 |
64,46 |
74,8 |
61,5 |
2,03 |
0,43 |
0,38 |
|
NLR |
>2,84 |
75,21 |
62,65 |
74,6 |
63,4 |
2,01 |
0,40 |
0,39 |
|
PLR |
>140,6 |
65,70 |
51,81 |
66,5 |
50,9 |
1,36 |
0,66 |
0,21 |
Note: COV cut-off value; Sn sensitivity; Sp specificities; LR (+) likelihood ratio positive; LR (-) likelihood ratio negative; +PV positive predictive value; -PV negative predictive value; YI Youden Index.
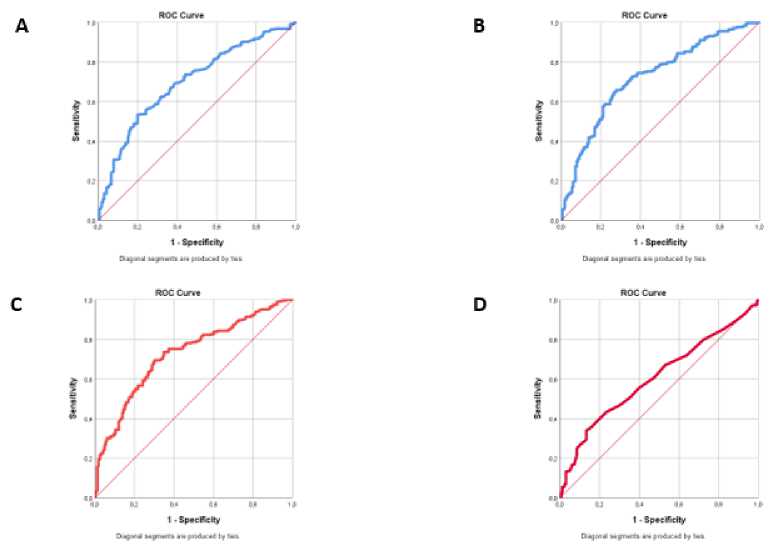
Figure 1. The ROC curve of Hematology parameters for diagnosing complicated appendicitis. A: WBC count, B: neutrophil count, C: Neutrophil-to-Lymphocyte Ratio (NLR), and D: Platelet-to-Lymphocyte Ratio (PLR).
DISCUSSION
In this study, the results showed that the Neutrophil-to-Lymphocyte Ratio (NLR) had the largest diagnostic ability among other hematological parameters for diagnosing complicated appendicitis (AUC 0.726; IK 0.677-0.775; p<0.0001). These results aligned with several studies with the same purpose. A study involved 1,597 patients undergoing appendectomy and compared the NLR values between the perforated appendicitis group and the acute appendicitis group (the cutoff point was 6.17, AUC 0.7 (0.63-0.77), p-value <0.001, sensitivity 76.32%, specificity 58.72%).11,12
Shashirekha et al. revealed that NLR could be one of the supporting parameters to diagnose perforated appendicitis, one aspect of complicated appendicitis. The systemic inflammatory response results in neutrophilia and lymphocytopenia, thus increasing NLR, which can be a marker for various abnormalities.13,14
The neutrophil count showed a fairly good ability, followed by leukocytes and PLR. The leukocyte count can be a significant parameter for diagnosing acute appendicitis.11 One study stated that the leukocyte count could help differentiate complicated and uncomplicated appendicitis. The study involved 425 patients with appendicitis. The cutoff values for leukocytes were 11.47, with a sensitivity of 71.9% and a specificity of 51.5%.15 These results have a sensitivity and specificity similar to ours, 73.55% and 56.02%, respectively.
To discriminate between uncomplicated and complicated appendicitis at the second diagnostic stage, excluding it is more critical than its inclusion. The clinician or surgeon should exclude complicated appendicitis if antibiotic treatment is considered. Therefore, the sensitivity and NPV values for detecting complicated appendicitis should be high.16
Several studies reported a significant increase in NLR in cases of acute appendicitis. The rise in NLR was also higher compared to
patients with complicated and uncomplicated appendicitis.16,17 NLR 4.68 can be a reasonably reliable parameter in diagnosing appendicitis, and NLR 5.74 can help differentiate between complex and uncomplicated appendicitis.17 Another study revealed that the cutoff value of 8.96 in the NLR can predict the occurrence of perforation in acute appendicitis. The results of the two studies differ from ours, with a cutoff value of NLR >2.84.
Laboratory tests greatly assist clinical decision-making when combined with signs and symptoms or radiological studies. A study of 845 people (mean age=11; the prevalence of acute appendicitis = 46.5%) found that even when the white blood cell count (WBC) was less than 10,000 per L (10.0 × 109 per L), 20% of patients still had acute appendicitis. However, in patients with equivocal ultrasound findings, a WBC count of less than 9,000 per L (9.0 × 109 per L) and less than 65% polymorphonucleocytes increased, and the negative predictive value increased from 41.9% to 95.8% (only 4,2% suffering from acute appendicitis).18
This study found that the characteristics of the male subjects are more than that of female subjects (52.2% vs. 47.8%). This result is similar to a study involving 67 complicated appendicitis patients and 106 uncomplicated patients, with 64.16% male subjects and 35.84% female subjects.19 Many studies also revealed more male appendicitis patients than women, and epidemiological data showed a ratio of 3:2.19,20 The median age of patients with appendicitis was 16 years (15 – 19) in this study, in line with several studies which revealed that acute appendicitis was most common in the young adult age group (60.3%).21
Our study found that the operative diagnosis of complicated appendicitis is higher than uncomplicated appendicitis
(59.31% vs. 40.69%). These results align with other studies, which showed a 59.67% result for the diagnosis of complicated appendicitis.22 The development from uncomplicated appendicitis to complicated appendicitis can be caused by various factors, such as limited access to health facilities, delays in examinations and logistical problems when referring patients. In addition, the behavior of delaying appendicitis patients decision to check their condition made it difficult for clinicians to determine the following treatment. Delay in diagnosing appendicitis can cause appendix complications into perforation, abscess formation, intra-abdominal adhesions, and sepsis.23 This study still has several limitations, such as unused medical record data because it lost some documents or was not stored correctly, causing us not to analyze the data obtained. In the future, similar research can be carried out with more detailed inclusion and exclusion criteria, increasing the number of subjects, or using different research methods. Thus, the outcome would have better and statistically meaningful data.
CONCLUSION
Hematological parameters: an increased number of leukocytes, neutrophils, monocytes, NLR, PLR, and a decreased number of lymphocytes can assist clinicians in diagnosing acute appendicitis, especially in establishing the operative diagnosis of complicated appendicitis. These parameters can also help clinicians or surgeons predict the severity of acute appendicitis, preventing delays in treating appendicitis patients. A hematological examination is a relatively easy test available in almost all hospitals, including the lowest type, in this case, type-C hospitals in Indonesia. Besides, this method is costeffective without budgeting for new modalities in hospitals/health services.
ACKNOWLEDGEMENT
The authors would acknowledge Aulia Azizah Mansyur, Izza Qorina, Adila Rahmia Nasuha, and Mochamad Fachraj Ar Razi for collecting data for this research. The author received a grant from the Ahmad Dahlan University Lecturer Research Scheme in 2021.
DISCLOSURE
None.
REFERENCES
-
1. Abdurachman S, Setiati S, Alwi I, et al. Apendisitis Akut Dalam: Ilmu Penyakit Dalam Jilid II. Comprehensive
Publications; 2016.
-
2. Sjamsuhidajat R JW de. Apendiks Veriformis. In: Buku Ajar Ilmu Bedah Edisi 4. Universitas Indonesia,
Directorate of Research and Public Service; 2017.
-
3. Choudhry AJ, Anandalwar SP, Choudhry AJ, et al. Uncovering Malpractice in Appendectomies: a Review of 234 Cases. Journal of Gastrointestinal Surgery. 2013;17(10):1796-1803.
-
4. Kabir SA, Kabir SI, Sun R, et al. How to diagnose an acutely inflamed appendix; a systematic review of the latest evidence. International Journal of Surgery. 2017;40(5):155-162.
-
5. Korkut M, Bedel C, Karancı Y, et al. Accuracy of Alvarado, Eskelinen, Ohmann, RIPASA and Tzanakis Scores in Diagnosis of Acute Appendicitis; a Cross-sectional Study. Archives of academic emergency medicine.
2020;8(1):e20.
-
6. D’Souza N, D’Souza C, Grant D, et al. The value of ultrasonography in the diagnosis of appendicitis. International Journal of Surgery. 2015;13:165-169.
-
7. Andersson REB. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. British Journal of Surgery. 2003;91(1):28-37.
-
8. Andersson M, Andersson RE. The
Appendicitis Inflammatory Response Score: A Tool for the Diagnosis of Acute Appendicitis that Outperforms the Alvarado Score. World Journal of Surgery. 2008;32(8):1843-1849.
-
9. Goulart RN, Silvério G de S, Moreira MB, et al. Achados principais de exames laboratoriais no diagnóstico de apendicite aguda: uma avaliação prospectiva. ABCD Arquivos Brasileiros de Cirurgia Digestiva (São Paulo). 2012;25(2):88-90.
-
10. Zhou H, Xu J, Han J, et al. Evaluation of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios as Reliable Biomarkers for the Diagnosis of Perforated Acute Appendicitis: A
Retrospective case control study. Research Square. 2020.
-
11. Shashirekha C, Singh R, Sanganboina S, et al. Preoperative neutrophil-to-
lymphocyte ratio in predicting the severity of appendicitis: A retrospective cohort study in a tertiary rural hospital. International Journal of Surgery Science. 2017;1(1):3-6.
-
12. Ahmad KA, Ideris N, Aziz SHSA. A Cross-Sectional Study of Neutrophil-to-Lymphocyte Ratio in Diagnosing Acute Appendicitis in Hospital Melaka. The Malaysian journal of medical sciences : MJMS. 2019;26(6):55-66.
-
13. Li MX, Liu XM, Zhang XF, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: A systematic review and meta-analysis. International Journal of Cancer.
2014;134(10):2403-13.
-
14. Wang X, Zhang G, Jiang X, et al. Neutrophil to lymphocyte ratio in relation to risk of all-cause mortality and cardiovascular events among patients undergoing angiography or cardiac revascularization: A meta-analysis of observational studies. Atherosclerosis. 2014;234(1):206-213.
-
15. Celik M, Tekin E, Bayraktar M. Use of platelet large cell ratio as a new biomarker in the diagnosis of acute appendicitis. Journal of Surgery and Medicine. 2020;4(6):479-82.
-
16. Bom WJ, Scheijmans JCG, Salminen P, et al. Diagnosis of Uncomplicated and Complicated Appendicitis in Adults. Scandinavian journal of surgery. 2021;110(2):170-179.
-
17. Kahramanca Ş, Özgehan G, Kaya O, et al. Platelet to Lymphocyte Ratio and Acute Appendicitis. Kafkas Journal of Medical Sciences. 2017;7(2):153-157.
-
18. Snyder MJ, Guthrie M, Cagle S. Acute Appendicitis: Efficient Diagnosis and Management. American family physician. 2018;98(1):25-33.
-
19. Rahman R, Kartini A, Widaningsih Y, et al. Analysis of Hematologic Parameters and Serum Bilirubin Levels in Complicated and Uncomplicated Acute Appendicitis Patients. Indonesian Journal Of Clinical Pathology And Medical Laboratory. 2020;26(2):229-234.
-
20. Toktaş O, Aslan M. Mean platelet volume, red cell distribution width,
neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in the diagnosis acute appendicitis. Eastern Journal Of Medicine. 2017;22(1):5-9.
-
21. Lima AP, Vieira FJ, Oliveira GP, et al. Clinical-epidemiological profile of acute appendicitis: retrospective analysis of 638 cases. Revista do Colégio Brasileiro de Cirurgiões. 2016;43(4):248-253.
-
22. Kong VY, Sartorius B, Clarke DL. Acute appendicitis in the developing world is a morbid disease. Annals of the Royal College of Surgeons of England.
2015;97(5):390-395.
-
23. Brown TW, McCarthy ML, Kelen GD, et al. An Epidemiologic Study of Closed Emergency Department Malpractice Claims in a National Database of Physician Malpractice Insurers. Academic Emergency Medicine. 2010;17(5):553-
560.
7

Discussion and feedback