Clinico-Pathological Characteristics of Penile Cancer Patients at Sanglah General Hospital Denpasar, Bali between 2013-2020
on

DIRECTORY OF
OPEN ACCESS
JOURNALS
P-ISSN: 2548-5962
E-ISSN: 2548-981X

Clinico-Pathological Characteristics of Penile Cancer Patients at Sanglah General
Hospital Denpasar, Bali between 2013-2020
I Gusti Ngurah Agung Indra Suharta1, I Wayan Yudiana2*, Anak Agung Gde Oka2
-
1 General Surgery Training Programme, Medical Faculty of Udayana University/Sanglah General Hospital, Denpasar, Bali, Indonesia.
-
2 Urology Department, Medical Faculty of Udayana University/Sanglah General Hospital, Denpasar, Bali, Indonesia.
*Corresponding author: yanyud@yahoo.com.
ABSTRACT
Aim: To know prevalence and clinico-pathological characteristic of penile cancer patients at Sanglah General Hospital Denpasar between 2013 until 2020 or for 7 years periode. Methods: A cross-sectional study to collect retrospective data of penile cancer patients at Sanglah Genaral Hospital from medical records between August 2013 until August 2020. Demographics data consisted of age group and patient’s origin, meanwhile histopathological data included pathological staging, histological subtype, grading, and lymphovascular invasion. Results: 96 penile cancer patients were collected for 7 years. The highest incidence was in 2020. Mean age was 57.60 ± 12.28 years old which dominantly in 60–69 years old groups. Most of patients origin from the rural area. The highest proportions were T3 stage (41,7%), N0 stage (38,5%), M0 stage (94,7%), SCC subtype (89,6%), G2 grade (71,9%), and LVI negative (65,4%). Conclusion: The prevalence of penile cancer patients are fluctuating but tended to increase since 2017. The peak incidence was in 60-69 years old group and from the rural area. Based on TNM staging system, the highest proportion was T3, N0, M0 and G2.
Keywords: penile cancer, characteristics, staging system.
DOI: https://doi.org/10.24843/JBN.2024.v08.i01.p05
INTRODUCTION
The incidences of penile cancer are rare in the world. In developed countries, the incidence of penile cancer was estimated less than 1% of all the malignancy cases in males, but the incidence is high enough in developing countries. Penile cancer cases are 1: 100,000 males in Amerika in 2000. This number already decreased in the 2014 to be 0.4–0.6 per 100,000 males. Meanwhile, in the developing countries such as Africa, South Amerika and some of Asia, the cases was high and very variated, about 8 – 10 per 100,000 males.1,2
The incidence rate of penile cancer in Indonesia was still low, except in some areas such as North Sumatra, Jakarta, Solo,
Yogyakarta, and Bali. The study by Digambiro et al. in H. Adam Malik Hospital Medan North Sumatra reported that in 5 years period of time (2008–2012), there were 30 penile cancer patients mostly from the age group of 50 – 59 years old.3 The other study in Cipto Mangunkusumo Hospital Jakarta and Kanker Dharmais Hospital Jakarta for 12 years (1994 – 2005) reported 69 penile cancer patients or 5.75 cases per year.4 Another study by Prayoga et al. at Sardjito Hospital Yogyakarta found 35 penile cancer cases or 4.3 cases per year in 8 years (2006 – 2013).5 The data in Bali based on 3 studies in Sanglah Hospital Denpasar in different periods (2001–
29 | JBN (Jurnal Bedah Nasional)
2015) reported the highest prevalent of penile cancer patients in Indonesia.6,7,8
There is no prevalence data of penile cancer in the last few years in Indonesia especially in Bali yet, so the latest descriptive study needs to be done to know about the characteristic of demograpic and clinical-histopathological features of penile cancer patients which came to Sanglah General Hospital Denpasar Bali.
METHODS
This study was a descriptive cross-sectional study to know the characteristic of penile cancer patients who came to Sanglah Hospital Denpasar Bali from August 2013 until August 2020. The penile cancer patient who get therapy at Sanglah Hospital Denpasar Bali from August 2013 until August 2020 with a varied stage which already proven by histopathology by surgery procedure and/or biopsy in the primary tumor or inguinal lymph gland was included. The sample is excluded if the medical record data is incomplete. The sample was collected by the consecutive sampling method.
The data was collected using secondary data from the medical record. Medical record data will be extracted using the collecting data form. The demography aspects were aged based on the ID card and place of origin data was classified to be urban area (town) and rural area (village). Clinical-histopathological aspects are penile cancer TNM stage (Tumor, Nodule, Metastasis), histology subtype, and penile cancer histology level based on the classification of AJCC 8th edition 2016, and lymphovascular invasion (LVI) features in the result of immunohistochemical stains.
The variables with nominal and ordinal data will be analyzed by demonstrating absolute numbers and percentages from each variable and cross-tabulation data. The
distribution of numeric data was calculated using Kolmogorov-Smirnov test. Data will be distributed normally if the p-value>0,05. The numeric data with normal distribution was presented as mean±standard deviation and not normal data was presented as median (minimum-maximum).
RESULTS
In the last 7 years (August 2013 - August 2020), there were 96 cases of penile cancer patients who came to Sanglah Hospital Denpasar with an average number of 13,7 cases per year. Annualy, the case was fluctuating, with the lowest prevalence in 2017 and the highest prevalence in 2020. The mean age of a penile cancer patient was 57.60±12.78 years old with the highest proportion in the age group 60-69 years old. Most of the cases was from a rural area (64.6%) (Table 1).
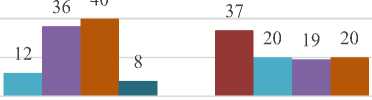
Tumor stage (T) and nodule (N), as pathological stage, were defined after the surgical and/or biopsy procedure, meanwhile clinical stage metastasis (M) were defined using radiology examination. The stage with the highest proportion was pT3 (41.7%), followed by pT2 (37.5%), pN0 (38.5%), and M0 (94.7%). The complete data can be seen in Figure 1.
Based on the histopathological features and examination, the highest proportion was usual SCC subtype (89.6%), followed by Warty type (7.3%) and Verucous type (3.1%). Based on histologic grading parameter, moderately differentiated or G2 was found as the highest proportion (71.9%), followed by well-differentiated or G1 (20.8%) and poorly differentiated (7.3%). Based on lymphovascular invasion (LVI) status, negative LVI was the most common (65.6%). The complete features can be seen in the Figure 2 (2a, 2b, and 2c).
Table 1. Demographic Distribution of Penile Cancer Patient at Sanglah General Hospital Denpasar since August 2013 until August 2020 (n = 96)
|
Variable |
Total |
Proportion (%) |
|
Years | ||
|
2013 |
16 |
16.7 |
|
2014 |
8 |
8.3 |
|
2015 |
13 |
13.5 |
|
2016 |
8 |
8.3 |
|
2017 |
5 |
5.2 |
|
2018 |
7 |
7.3 |
|
2019 |
14 |
14.6 |
|
2020 |
25 |
26.0 |
|
Total |
96 |
100 |
|
Age | ||
|
Range (years) |
35 – 91 | |
|
Mean ± SD (years) |
57.60±12.78 | |
|
Age Group | ||
|
<40 years old |
8 |
8.3 |
|
40 – 49 years old |
18 |
18.8 |
|
50 – 59 years old |
28 |
29.2 |
|
60 – 69 years old |
29 |
30.2 |
|
≥70 years old |
13 |
13.5 |
|
Total |
96 |
100 |
|
Place of Origin | ||
|
Urban |
34 |
35.4 |
|
Rural |
62 |
64.6 |
|
Total |
96 |
100 |
Penile Cancer Staging
100
80
3 60
O
H 40
20
0
pT1 pT2 pT3 pT4
pN0 pN1 pN2 pN3
Staging
91
5
■0
■1
■2
■3
■4
M0 M1
Figure 1. Graphic of Penile Cancer Patient Stage (TNM) in Sanglah Hospital Denpasar since August 2013 until August 2020 (n=96)
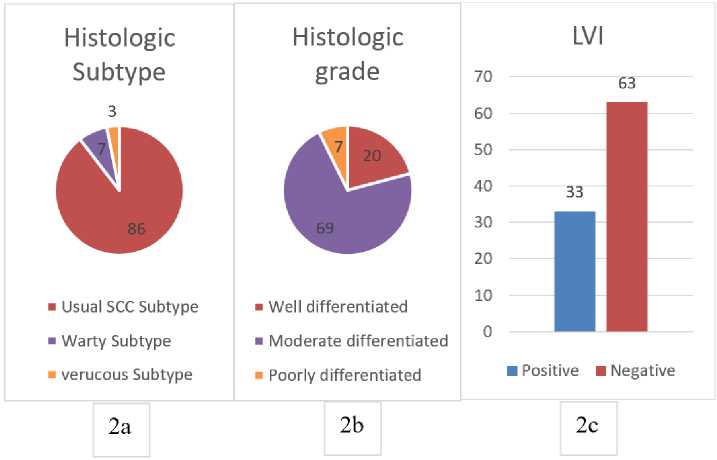
Figure 2. The graphic result of histopathology examination which is defined of Histologic subtype (2a), Histologic grade (2b), and Lymphovascular Invasion (LVI) of penile cancer patient in Sanglah hospital Denpasar since August 2013 until August 2020 (n=96).
Table 2 and Table 3 described the crosstabulation between the aged group and place of origin group with the TNM stage. The under 60 years old group tend to have a higher tumor stage (T3) compared to above 60 years old group (T2). As well as the regional nodule stage, under 50 years old group tend to have
the higher stage (N2-3) compared to the above 50 years old group (N0-1). Based on variable place of origin, patient from urban areas tend to have penile cancer in the early stage (T2, N0-1) compared to rural areas (T3, N0-3), and metastases positive (M1) patients was mostly from rural areas.
Table 2. Cross tabulation result of aged and place of origin group by T stage and N penile cancer stage in Sanglah Hospital Denpasar since August 2013 until August 2020.
|
Variable |
Staging T n(%) pT1 pT2 pT3 pT4 Total |
|
Aged group <40 (years old) 40 - 49 50 - 59 60 - 69 ≥70 |
0 (0) 2 (25.0) 5 (62.5) 1 (12.5) 8 (100.0) 1 (5.6) 7 (38.9) 10 (55.6) 0 (0) 18 (100.0) 6 (21.4) 9 (32.1) 11 (39.3) 2 (7.1) 28 (100.0) 4 (13.8) 11 (37.9) 9 (31.0) 5 (17.2) 29 (100.0) 1 (7.7) 7 (53.8) 5 (38.5) 0 (0) 13 (100.0) |
|
Place of Urban origin Rural |
4 (11.8) 14 (41.2) 13 (38.2) 3 (8.8) 34 (100.0) 8 (12.9) 22 (35.5) 27 (43.5) 5 (8.1) 62 (100.0) |
|
Variable |
Staging N n(%) pN0 pN1 pN2 pN3 Total |
|
Aged group <40 (years old) 40 - 49 50 - 59 60 - 69 ≥70 |
2 (25.0) 0 (0.0) 1 (12.5) 5 (62.5) 8 (100.0) 5 (27.8) 3 (16.7) 7 (38.9) 3 (16.7) 18 (100.0) 13 (46.5) 4 (14.3) 5 (17.9) 6 (21.4) 28 (100.0) 12 (41.4) 8 (27.6) 3 (10.3) 6 (20.7) 29 (100.0) 5 (38.5) 5 (38.5) 3 (23.1) 0 (0.0) 13 (100.0) |
|
Place of Urban origin Rural |
37 (41.2) 9 (26.5) 8 (23.5) 3 (8.8) 34 (100.0) 23 (37.2) 11 (17.7) 11 (17.7) 17 (27.4) 62 (100.0) |
Tabel 3. Cross tabulation aged and place of origin group with penile cancer patient based on stage M in Sanglah Hospital Denpasar since August 2013 until August 2020.
|
Variable |
Staging M, n(%) | |||
|
M0 |
M1 |
Total | ||
|
Aged group |
<40 |
8 (100.0) |
0 (0.0) |
8 (100.0) |
|
(years old) |
40 – 49 |
17 (94.4) |
1 (5.6) |
18 (100.0) |
|
50 – 59 |
25 (89.3) |
3 (10.7) |
28 (100.0) | |
|
60 – 69 |
28 (96.6) |
1 (3.4) |
29 (100.0) | |
|
≥70 |
13 (100.0) |
0 (0.0) |
13 (100.0) | |
|
Place of |
Urban |
60 (96.8) |
2 (3.2) |
34 (100.0) |
|
origin |
Rural |
31 (91.2) |
3 (8.8) |
62 (100.0) |
DISCUSSION
There is some study that reported the prevalence of penile cancer cases, especially in Indonesia. A study by Sugandi in Bandung - West Java report that penile cancer prevalence about 6% from all cancer patients in Hasan Sadikin Hospital Bandung.9 A study in Jakarta which involved 2 Central hospitals (referral center hospitals) reported the increase of penile cancer cases from an average of 3.6 cases per year to 5.7 cases per year in the early 20th century.4 Another study in Yogyakarta reported 35 penile cancer cases in 8 years or the average of 4.3 cases per year; in Medan – North Sumatra 30 cases in 5 years or the average of 6 cases per year.3,5
In Bali, some studies about penile cancer has been done in different periods. The study by Sastrodihardjo et al in Sanglah Hospital Denpasar reported 72 penile cancer cases in 12 years (April 1993–May 2005) or an average of 6 cases per year.6 A study by Theddy et al also reported 57 penile cancer cases in 5 years (2010–2014) or an average of 11.4 cases per year.7 Another study by Yudiana et al found 65 penile cancer cases in 5 years or an average of 13 cases per year.8 Meanwhile, this study found 96 penile cancer cases in the last 7 years, or an average of 13.7 cases per year. This prevalence clearly showed that there are an increase in penile cancer cases in Bali from year to year and the most cases in Indonesia if
compared to the last study or study in another area.
The incidence of penile cancer increases with age, and the peak is in the 6th – 7th decade, but can also happen in younger males. The increase of the incidence which is in line with aging does not exclude the role of somatic mutation accumulation which triggers the carcinoma cell formed, starting from the irritation process, inflammation, and infection chronically or in years.10 The average age of penile cancer patients in this study was 57.60 ± 12.78 years old with the most cases in group 60 -69 years old. This result is in line with the study by Sastrodihardjo et al which found the average age of penile cancer patients was 54.5 ± 14.6 years old with the youngest age being 27 years old and the oldest age being 100 years old.6 A study by Prayoga et al also showed the average age was 56 ± 14.4 years old, but they found more in the group of age 40-60 years old.5 The great proportion number in the group of 60 – 69 years old also in line with the study by Theddy et al which reported 36,8% penile cancer cases in group older than 60 years old and study by Yudiana et al which found the average age was 53.24 ± 13.42 years old with the youngest was 27 years old and the oldest was 86 years old.7,8 Different result was reported in a study by Tranggono et al which found the average age of penile cancer patients was 48.75 ± 15.47 years old with the age range being 40–50 years old.4
Based on TNM stage, in this study, most of the penile cancer patients which came to Sanglah Hospital Denpasar was in pT3 stage. This result is similar to the study by Prayoga et al which reported pT3 and pN0 stage was the dominant stage of the penile cancer patient in Yogyakarta, but for the metastases variable was still undiagnosed (cMx).5 A study in Jakarta reported most of the patients was in pT1 stage and pT2.4
Based on the histopathology subtype, the usual squamous cell carcinoma type is the most common. In this study, it was dominated by the usual SCC, followed by wart subtype and verrucous which have the same good prognosis. Similar results were reported in a study by Tranggono et al in Jakarta with the usual SCC histopathology sub-type was about 86.9% and a study by Yudiana et al with the prevalence of usual SCC histopathology subtype was about 90%.4,8
The study result also compared penile cancer patients' place of origin with a bigger proportion in the rural area (64.6%) compared to in the urban area (35.4%). It can be understood because the patient who lives in the rural area didn’t understand the risk factors and the prevention of penile cancer yet, especially about circumcision and external genitalia hygiene. Also, their understanding of the importance of early screening of cancer is very limited, so they generally come to the doctor in the late stage. In this study, the most of the patient from rural area was diagnosed in the T3 and N0-3 stage. Patients from rural area also had higher proportion of positive metastases (M1) cases than patients from urban area.
Histological grade of penile cancer was dominated by moderately differentiated which followed by well-differentiated. It is possibly related to the histology subtype which has the good prognosis. This result has also been found in the study by Yudiana et al which 69%
penile cancer was at the moderate level (G2).8 The different result was reported by Tranggono et al which found a good differentiated level (G1) as a dominant cases.4
Lymphovascular invasion (LVI) already known as the predictive factor of the metastases inguinal lymph gland in penile cancer for a long time, besides the stage and primary tumor histologic grade. In this study, about 65,6% of cases with negative LVI, with nodule negative (N0) was the highest proportion. Study by Li et al reported the same result that negative LVI cases was more common than positive LVI patients. The positive LVI group was found to have a significant lower overall survival (OS) than the negative LVI group.11
CONCLUSION
The prevalences of penile cancer in Sanglah Hospital Denpasar are fluctuating but tended to increase in the last 5 years. Most cases of penile cancer is in 60-69 years old and from rural area. The most histopathology characteristic is the usual SCC subtype, with primary tumor stage pT3 and pT2, G2, and also negative LVI.
DECLARATIONS
All the writers have no conflict of interest in this study publication
FUNDING
This study is using personal funding by the writers.
REFERENCES
-
1. Douglawi A, Masterson TA. Updates on the epidemiology and risk factors for penile cancer. Transl Androl Urol. 2017;6(5):785-790.
-
2. Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9-29.
-
3. Digambiro RA, Alferally I, Delyuzar. Hubungan Antara Derajat Histopatologi Karsinoma Penis dengan Tampilan 8.
Imunohistokimia HER-2. Majalah
Patologi. 2016;25(2):24-28.
-
4. Tranggono U, Umbas R. Karakteristik dan Terapi Penderita Keganasan Penis di RS Cipto Mangunkusumo dan RS Kanker "Dharmais". Indonesian Journal of 9. Cancer. 2008;2(2):45-50.
-
5. Prayoga DA, Tranggono U. Evaluasi Klinis dan Manajemen Kanker Penis di 10. Rumah Sakit Sardjito, Yogyakarta. Indonesian Journal of Cancer. 2015;10(1):29-34.
-
6. Sastrodihardjo B, Duarsa GWK, Partama IPG. Hubungan Ekspresi p-53 dengan Gambaran Kinikopatologi pada Penderita 11. Karsinoma Penis yang Dirawat di Rumah Sakit Sanglah, Denpasar (2001-2005). Indonesian Journal of Cancer. 2009;3(3):85-90.
-
7. Theddy H, Yudiana IW, Oka AAG. Karakteristik Pasien Karsinoma Penis di
Rumah Sakit Sanglah Tahun 2014. MEDICINA. 2018;49(2):48-51.
Yudiana IW, Harmaya AK, Oka AAG, Djatisoesanto W. Predictive Factors Of Inguinal Lymph Node Metastasis In Men With Penile Cancer At Sanglah Hospital, Denpasar, Bali. Dermatology Reports. 2019;11(s1):8046.
Sugandi S. Referral Pattern of Urological Malignancy in Indonesia. Br J Urol. 1989;63(1):1-3.
Hansen BT, Orumaa M, Lie AK, Brennhovd B, Nygård M. Trends in incidence, mortality and survival of penile squamous cell carcinoma in Norway 1956-2015. Int J Cancer. 2018;142(8):1586-1593.
Li K, Sun J, Wei X, et al. Prognostic value of lymphovascular invasion in patients with squamous cell carcinoma of the penis following surgery. BMC Cancer. 2019;19(1):476.
35
Discussion and feedback