Retroperitoneal Pleomorphic Rhabdomyosarcoma in Adult: A Rare Case Report
on

Retroperitoneal Pleomorphic Rhabdomyosarcoma in Adult: A Rare Case Report
Budi Martono1*, Sri Inggriani2
-
1 Staff of Emergency Department, Medistra Hospital, Jakarta.
-
2 Head of Radiology Department, Medistra Hospital, Jakarta.
*Penulis korespondensi: budimartono89@gmail.com.
ABSTRACT
Background: Rhabdomyosarcoma (RMS) is the most common type of soft tissue sarcoma in children, however, RMS is a rare malignancy in adults. Head and neck are the most common site for RMS, while intrabdominal RMS are rare in adults. Case: We present a rare case of a retroperitoneal abdominal mass, treated surgically with histopathology results of a retroperitoneal RMS. We discuss the clinical presentation, image findings, and treatment for this case. Conclusion: Intraabdominal tumours need to be identified quickly and precisely. CT scan or MRI can help clinicians to determine the staging, therefore plans the best treatment for the patient. In our case, surgery and radiotherapy showed promising outcome. The lack of literature and consensus on a standardized approach to systemic treatment and outcome in retroperitoneal pleomorphic RMS in adults makes our case a rare presentation of rhabdomyosarcoma and thus the need for reporting.
Keywords: rhabdomyosarcoma, retroperitoneal, pleomorphic.
DOI: https://doi.org/10.24843/JBN.2020.v04.i02.p04
INTRODUCTION
Soft tissues sarcomas make up >1% of all adult malignancies and RMS is only represent 3% from these soft tissue sarcomas.1 Rhabdomyosarcoma is a highly malignant mesenchymal tumour, originating from immature striated muscle.2 Usually RMS can be discovered as a tumour in the head and the neck (35%), the genitourinary tract (22%), and other extremities (18%). There are four different sub-types of RMS defined by WHO classification by their histologic features: embryonal, alveolar, pleomorphic and spindle cell/sclerosing.3 The histologic distribution of RMS differs in adults than young children.4 The pleomorphic subtype is more often encountered in adult patients and also carries the worst prognosis.2,5
CASE REPORT
A 46 years old Indonesian male, came with complaint of change in urinating frequency
followed by palpable mass growing on his left lower abdomen within 1 month prior of examination. On physical examination, we found a palpable mass on the left lower quadrant, no tenderness, with size of 10 cm, smooth surface, firm consistency, and immobile. His blood laboratories are within normal limit. Lower abdominal ultrasound showed solid mass on the left pelvic side near the bladder with size measuring ± 9.93 cm x 11.15 cm x 11.55 cm and spot of vascularity intra-tumour on Colour Doppler Sonography while kidney, bladder and prostate within normal (Figure 1).
Abdominal CT (computed tomography) scan with contrast showed solid, smooth bordered, hyper-vascular mass, which show fine septation intratumor, seen located in the left hemi pelvis, measures 12.6 cm x 12.1 cm x 10.9 cm, and has a feeding artery originating from the aorta abdominal-infrarenal level (Figure 2).
62 | JBN (Jurnal Bedah Nasional)
No calcification is seen intratumor. The tumour caused a superior displacement of the sigmoid, caudal-medial warts of the tumour reaches until the level of upper bladder; the posterolateral part of the tumour reaches until the left iliopsoas margin. No peritumoral fat infiltration is seen in the surrounding tumour. There is no liver mass/ metastasis seen. No pathological lymph nodes metastasis in the pelvis nor retroperitoneal. The mass is suspected as a sarcomatous tumour or GIST (gastrointestinal stromal tumor). Upon Imaging results, we conclude the patient to have a stage 3 tumour (staging of T2bN0M0 using the TNM classification).
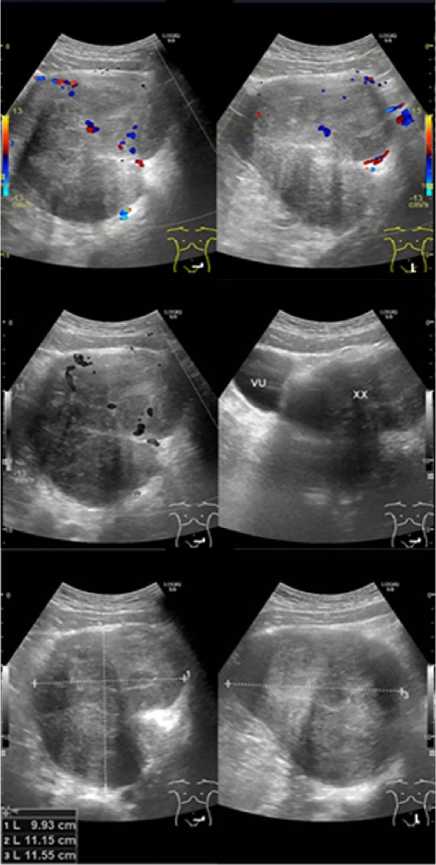
Figure 1. Abdominal Ultrasound.

Figure 2. Abdominal CT scan with contrast showed show solid, smooth bordered, hyper-vascular mass, which show fine septation intratumor, seen located in the left hemi pelvis, and has a feeding artery originating from the aorta abdominal-infrarenal level (green arrow).
The patient then undergoes laparotomy surgery, the patient was put under general anaesthesia, when the peritoneum was seen, the tumour is located at the left extraperitoneal pushing the sigmoid. Then the tumour was freed from its surrounding. There is an injury to the sigmoid serosa upon freeing the tumour, however it did not perforate the sigmoid which then repaired with suture, bleeding was controlled then the surgery site was then
closed. Macroscopically the mass is 14 cm x 10 cm x 8 cm, located retroperitoneal, with smooth margin, and easily distinguished from adjacent structure.

Figure 3. Macroscopically feature of the mass.

Figure 4. PET scan after surgery.
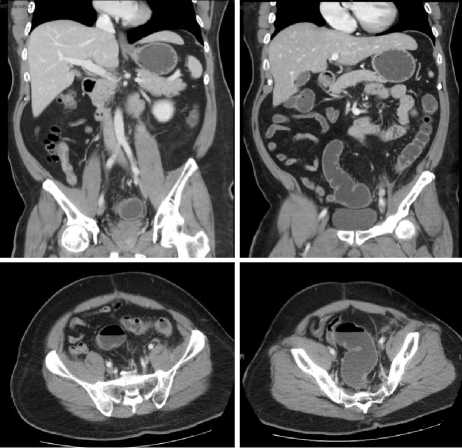
Figure 5. Abdominal CT scan follow up 5 months after surgery, showed no visible mass and no residual tumour at the left pelvic.
The histopathological exam showed a tumour mass with defined border, with bundled spindle cell, hyperchromatic nuclei with some of them shaped bizarrely, and multi nucleated with mitosis 4/50 high-power fields. There is no invasion of lympho-vascular and necrosis seen. Immunohistochemistry (IHC) shows, CD 117 negative, S100 negative, SMA and vimentin is positive on the spindle cell, negative on the pleomorphic cells. Desmin and MyoD1 is positive on both spindle cell and pleomorphic cells. The IHC supported the diagnosis of pleomorphic rhabdomyosarcoma.
PET (positron emission tomography) scan was performed 2 months after surgery, it showed hypermetabolic lymph nodes enlargement at left external iliac suspect of metastatic process (Figure 4). At the left intra cavum pelvic, obscure area was seen with mild metabolic activity at the area post-surgery, might be caused due to inflammation postsurgery or residual mass.
The patient then was consulted with oncologist and which then scheduled for radiation therapy and finished the radiation course without any complications. 5 months
after radiation therapy, the patient underwent another CT abdomen with contrast, which showed no visible mass and no residual tumour at the left pelvic while other abdomen organs are normal (Figure 5). The patient is now currently well and actively working while still scheduled for periodic observation.
DISCUSSION
Most of the retroperitoneal neoplasms are malignant.16 Usually, when they present clinical manifestation, it presents as a large mass tumour and involved surrounding
organs.11 RMS usually comes from immature mesenchymal cells that relates to skeletal muscle lineage, but these tumours can grow in tissues in places where striated muscle is not normally found.17 Retroperitoneal pleomorphic rhabdomyosarcoma (PRMS) in adult is extremely rare and also malignant. We searched for relevant literature of similar cases, however we found only a few case reports written in English that describe primary retroperitoneal pleomorphic RMS (Table 1).5
Table 1. Reported Cases of Retroperitoneal Rhabdomyosarcoma.
|
Age |
Histology |
Metastasis |
Treatment |
Prognosis | ||||
|
No |
Reference |
(y) |
Sex |
Presentation | ||||
|
1 |
Kumar et al.6 |
61 |
M |
Lump, burning pain |
Spindle cell |
NA |
Inoperable, Chemotherapy |
NA |
|
2 |
Yadav et al.7 |
65 |
M |
Abdominal pain, vomiting, obstipation |
Embryonal |
NA |
Inoperable, conservative |
NA |
|
3 |
Qadri et al.8 |
50 |
M |
Mass, constipation |
Pleomorphic |
Inguinal lymph node |
Surgery, radiotherapy, chemotherapy |
Died (<3 mo) |
|
4 |
Furlong et al.2 |
32 |
M |
NA |
Pleomorphic |
NA |
NA |
Died (1 y) |
|
5 |
Furlong et al.2 |
58 |
M |
NA |
Pleomorphic |
NA |
NA |
Died (1 y) |
|
6 |
Furlong et al.2 |
81 |
F |
NA |
Pleomorphic |
NA |
NA |
Died (1.5 y) |
|
7 |
Furlong et al.2 |
64 |
M |
NA |
Pleomorphic |
NA |
NA |
Died (2 mo) |
|
8 |
Yu et al.10 |
37 |
F |
Mass |
Spindle cell |
NA |
Surgery |
NA |
|
9 |
Martono et al.* |
46 |
M |
Mass, increase urine frequency |
Pleomorphic |
Left external iliac lymph node |
Surgery, radiotherapy |
No evidence of disease |
*note that the 9th case is the current case report. M = male; F = female; y = years; mo = month; NA = not available.
In a study performed by Furlong et al., PRMS is mentioned as a rare variant of RMS that almost always occurs in adults, with mean
age of 49 years and has a very poor prognosis.2 In our case, we also found similarities with
these findings. The tumour is often large (>10 cm), and mostly fleshy, well-circumscribed.
Patient usually present without complaints such as pain, unless it is related to the mass effect or pain can be caused by complications that are secondary to the organs around the tumour (e.g. intra-abdominal tumours may present with bowel obstruction or compression upon adjacent neural structures). Therefore, imaging studies should include CT scan or MRI (magnetic resonance imaging) targeting the primary tumour to determine the size and possible involvement of other vital organ around the primary tumour; as findings in imaging studies can help surgeons in planning surgical resection.10 Usually, RMS in CT scan or MRI shows as a mass lesion with areas of calcification, necrosis, and heterogeneous enhancement, with high-flow blood vessels in the tumor.11
Understanding role of CT scan is important, in our case, from CT findings we can locate that the mass is at retroperitoneal space, it was seen located in the left hemipelvis, that cause a superior displacement of the sigmoid, pressing the upper part of bladder, and left iliopsoas margin as it’s posterior margin, and has feeding artery origin from the infrarenal level of abdominal aorta. These findings can help surgeon to determine the staging and plan the easies access to the mass. Figure 6 showed how to evaluate intraabdominal lesion whether it’s a retroperitoneal or intraperitoneal tumour.
Pleomorphic rhabdomyosarcoma can be distinguished from embryonal and alveolar RMS based on histomorphology. Normally, on microscopic examination the tumour cells are seen to be arranged in sheets and lobules. Cells are pleomorphic, with round to elongated nuclei and abundant eosinophilic cytoplasm. However, it could easily be confused with undifferentiated high-grade pleomorphic sarcoma (malignant fibrous
histiocytoma) that is why IHC analysis plays an important role to address specific skeletal muscle markers and nonspecific myoid markers for achieving the diagnosis of PRMS.8,9 RMS in IHC analysis shows high sensitivity and specificity for MyoD1 and/or myogenic positive which shows distinction from other adult pleomorphic soft tissue sarcomas.12 The histopathologic findings in our case is positive immunoreactivity to desmin and MyoD1 antibodies, therefore it is concluded to be a PRMS.
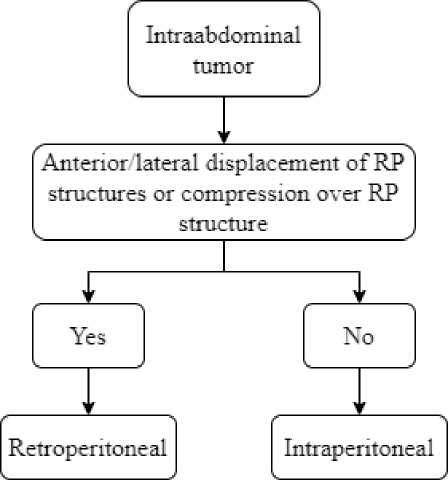
Figure 6. Step to identify the lesion whether its intra or retroperitoneal (RP).18
Due to the rarity of the case, there is little information on the management and prognosis of the patient. Current guidelines for treating RMS in adult patients are based on the Intergroup Rhabdomyosarcoma Studies (IRS) which is based on treating children with RMS.13
There are three main choice of treating patients with RMS. These are surgery, radiation therapy (RT) and systemic combination chemotherapy.8 Surgery is the therapy of choice for adult RMS, as it seen to improved survival rate14. In IRSG protocols,
all RMS patient should get RT in order to control the tumour locally in case of any residual tumour after surgery.15In our case, the patient undergo surgery with radiotherapy post-surgery which showed promising result. Patient follow-up plan is with a PET scan examination 6 month after surgery and 12 months after, once ensured there is no residual mass.
CONCLUSION
Intraabdominal tumour needs to be identified quickly and precisely. CT scan or MRI can help clinicians to determine the staging, therefore plans the best treatment for the patient. In our case, from histopathology results was confirmed to be PRMS which is a malignant tumour with poorer outcome in adults than in paediatric population. However, it seems that in our case, with surgery and radiotherapy the patient showed promising outcome. We conclude that treatment of retroperitoneal PRMS in adults should follow the treatment standard of PRMS in paediatric case until more cases have been evaluated or an adult adjusted guideline is available.
The lack of literature and consensus on a standardized approach to systemic treatment and outcome in retroperitoneal pleomorphic RMS in adults makes our case a rare presentation of rhabdomyosarcoma in adults and thus the need for reporting.
CONFLICT OF INTEREST
We declare no conflict of interest.
REFERENCE
-
1. Weiss SW, Goldblum JR, Folpe AL. Enzinger and Weiss' soft tissue tumors, 5th edition. Philadelphia: Mosby; 2007. p.601-38.
-
2. Furlong MA, Mentzel T, Fanburg-Smith JC. Pleomorphic rhabdomyosarcoma in adults: A clinicopathologic study of 38
cases with emphasis on morphologic variants and recent skeletal musclespecific markers. Mod Pathol. 2001;14:595-603.
-
3. Fletcher CDM, Bridge JA, Hogendoorn PCW, et al. WHO Classification of Tumors of Soft Tissue and Bone, 4th Edition, Volume 5. France: IARC Press; 2013. p.127-34.
-
4. Sultan I, Qaddoumi I, Yaser S, et al. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: an analysis of 2,600 patients. J Clin Oncol. 2009;27:3391-7.
-
5. Alkhormi AM, Alqifari A, Aljarbou OZ, et al. Primary duodenal embryonal rhabdomyosarcoma in adults: a case report. AME Case Rep. 2019;3:29.
-
6. Kumar H, Heroor A, Vanan A, et al. IntraAbdominal Retroperitoneal
Rhabdomyosarcoma in Adult: A Rare Case Report & Review of Literature. IOSR Journal of Dental and Medical Sciences. 2017;16:36-8.
-
7. Yadav SK, Sinha DK, Ahmed A, Azhar T, et al. Primary Intra-Abdominal Rhabdomyosarcoma in an Adult: an Unusual Presentation and Review of Literature. Indian J Surg Oncol. 2015;6:119-22.
-
8. Qadri S, Alam K, Alam F. Retroperitoneal pleomorphic rhabdomyosarcoma
metastasizing to inguinal lymph node. Clin Cancer Investig J. 2015;4:404-7.
-
9. Yu L, Yang SJ. Spindle cell rhabdomyosarcoma of the
retroperitoneum: an unusual case
developed in a pregnant woman but obscured by pregnancy. Int J Clin Exp Pathol. 2014;7:4904-12.
-
10. Egas-Bejar D, Huh WW.
Rhabdomyosarcoma in adolescent and young adult patients: Current
perspectives. Adolesc Health Med Ther. 2014;5:115-25.
-
11. Rajiah P, Sinha R, Cuevas C, et al. Imaging of uncommon retroperitoneal masses. Radiographics. 2011;31:949-76.
-
12. Nakayama R, Nemoto T, Takahashi H, et al. Gene expression analysis of soft tissue sarcomas: Characterization and
reclassification of malignant fibrous histiocytoma. Mod Pathol. 2007;20:749-59.
-
13. Khosla D, Sapkota S, Kapoor R, et al. Adult Rhabdomyosarcoma: Clinical
Presentation, Treatment, and Outcome. J Cancer Res Ther. 2015;11:830-4.
-
14. Ferrari A, Dileo P, Casanova M, et al. Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients
treated at a single institution. Cancer. 2003;98:571-80.
-
15. Crist W, Gehan EA, Ragab AH. The third Intergroup Rhabdomyosarcoma Study. J Clin Oncol. 1995;13:610-30.
-
16. Neville A, Herts BR. CT characteristics of primary retroperitoneal neoplasms. Crit Rev Comput Tomogr. 2004;4:247-70.
-
17. Husband DJE, Reznek RH. Husband and Reznek's Imaging in Oncology, 3rd Edition. UK: Informa Healthcare; 2009. p.941-6.
-
18. Bhargavi DV, Avantsa R, Kala P. MDCT signs differentiating retroperitoneal and intraperitoneal lesions-diagnostic pearls. Electronic Presentation Online System. 2015:C-0987.
68

Discussion and feedback