Capillary-Cavernous Hemangioma of Lymph Node: An Extremely Rare Case
on
Capillary-Cavernous Hemangioma of Lymph Node: An Extremely Rare Case
I Gede Surya Dinata1*, Made Jatiluhur2
-
1 Faculty of Medicine, Universitas Pendidikan Ganesha, Buleleng, Bali, Indonesia.
-
2 Department of Pathology, Buleleng District Hospital, Buleleng, Bali, Indonesia.
*Corresponding author: surya.dinata@undiksha.ac.id.
ABSTRACT
Background: Hemangioma is a benign vascular tumour commonly found in young children. This tumor can grow within many organs, but occurring in the lymph node is extremely rare. The capillary-cavernous hemangioma (CCH) of the lymph node was mostly found as an incidental finding after histopathology confirmation of oncological surgery. Case: We presented the first case of intranodal CCH from the parietal region of the head in a 11-year-old boy. The easily-bleed lump was found above the head fascia and confirmed with histopathological examination. Conclusion: The capillary-cavernous hemangioma arising from the lymph node was an extremely rare pathological finding after oncological surgery. Treatment by surgical excision was curative. The awareness of this benign vascular tumour must be known to physicians so that it was not mistakenly diagnosed as a malignant disease with subsequent unnecessary radical therapy.
Keywords: hemangioma, CCH, lymph node.
DOI: https://doi.org/10.24843/JBN.2021.v05.i01.p04
INTRODUCTION
Hemangioma arising in lymph node was an extremely rare condition. In 1992, Chan et al. reported the first 39-case series of the primary vascular tumour of the lymph node, including hemangioma. They classified the hemangioma to five major groups: hemangioma, angiomatous hamartoma, epitheloid vascular, hemangioendothelioma, and lymphangioma.1 The last case report was done by Teseiras et al., in which they reported a case of the capillary cavernous type of hemangioma in the axilla region causing the symptom of pain in the shoulder.2
Hemangioma is the most frequent vascular tumor in children mostly found in skin and subcutaneous tissue,3 while occurrence in the lymph node is very rare.4 Recently, there were only 11 cases of capillary cavernous hemangioma (CCH) reported in the literatures.1,2,5-8 Most nodal CCH were
discovered as an incidental findings from a solitary lymph node enlargement in oncologic surgery.2 The most prevalence lymph node site is in the axilla and pelvic.1,2,5,6,8,9 New classification from the International Society for Study of Vascular malformations (ISSVA) in 2018, put it as a benign and fastflow vascular tumor.10,11 The correct diagnosis is often discovered until the results of histopathology examination.
CASE REPORT
We reported a case of intranodal CCH in a 11-year-old boy, who came to the hospital because of an occurrence of a painless lump in the parietal region of the scalp since 3 months ago. At first, the lump was as big as bean but then enlarge to about as big as peanut. The parents worried about the lump because of increasing size. On examination, we found a single discrete nodule, about 1,5
cm located subcutaneously, slightly mobile with a smooth surface, and non-tender. The skin overlying the nodule did not show any abnormality. There was no other tumor found in the head and neck and another region of the body. There were no family history of the same condition and the patient did not have a history of congenital disorder or syndrome. The blood sample taken did not reveal any abnormality. The patient was planned for an open biopsy procedure two days after the first visit.
During the operation, the nodule was found located above the fascia (galea), and appear white with a smooth surface, and easily dissected free from surrounding tissue. What came to attention was the bleeding seemed profuse when the nodule was dissected, even with the infiltration of the mixture of adrenaline and lidocaine before the incision. The bleeding came from the small vessels entering the node and must then be stopped by clamp and ligation. There was no other lymph node found during exploration of the surrounding tissue and the wound is closed primarily. The sample was taken then sent to the laboratory for histopathology examination.
The histopathology examination revealed a gross appearance showed the well encapsulated nodular mass measured 1x1x1 cm with grey to dark brown colour. Under low magnification, it showed a well-encapsulated nodular mass comprising of collagen stromal with lobules of small capillary and cavernous vessels and lymphoid follicle with the germinal center. The vessels were lined by flat to plump endothelial cells with red blood cells within the lumen. Almost half of the nodal parenchyma was effaced by the vascular lesion with the residual lymphoid aggregates underneath the capsule. The lobules of the vascular tumor were separated by collagenous stroma. There were
no areas of necrosis, cytological atypia or any atypical mitotic (Figure 1).
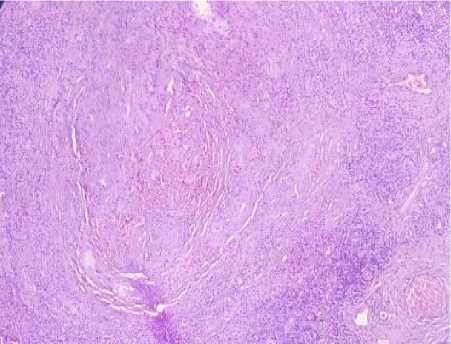
Figure 1. Microscopic appearance with HE stain (40x Magnification).
DISCUSSION
Since the first review of Chan et al.1 in 1992, the primary vascular tumour of the lymph node was still rarely encountered in clinical practice. Among other primary nodal vascular tumor, hemangiomas were extremely rare benign vascular tumors, which were usually asymptomatic. It could occur at any age, but mostly found in the middle-aged group (range 11-75 year-old, median 56 year.), with females predominant (3 vs. 8).1,2,5-9 Our case is the first case in which symptomatically enlarged lymph node in the parietal region of the head, below the scalp occurred in a 11-year-old boy and not associated with malignancies.
Four histologic types of intranodal hemangioma have been identified: capillary/cavernous, lobular capillary, cellular, and epithelioid with distinct microscopic features.4 Our case was capillary-cavernous hemangioma (CCH), which was the most commonly reported type. The tumor consisted of a solid, well-demarcated mass of proliferated capillary and cavernous vessels, covering almost half of the nodal parenchyma. Endothelial cells lining was flat and plumped filled with red blood
cells within the lumen. Hemangiomas of lymph node could occur at any lymph nodes of our body and usually only a single node involved, asymptomatic, and mostly found by incidental finding from surgeries from malignancies, as a part of the radical dissection.
In a review by Chan et al., CCH was diagnosed incidentally when lymph nodes are surgically removed, mostly from a radical mastectomy for breast cancer from the axilla or radical hysterectomy for endometrial adenocarcinoma from iliac nodes. It was also reported one case of symptomatic solitary enlargement of the supra-axilla lymph node.1 The microscopic appearance of capillary/cavernous hemangioma like our case was located more centered on the lymph node hilum or medulla with no destruction of nodal parenchyma. CCH characterized by a well-defined or poorly defined mass of capillaries or cavernous vessels with flat endothelial cells and can be empty or filled with blood. On the other hand, the lobular capillary type can almost replace the entire nodal parenchyma and resemble pyogenic granuloma. More solid structure with very few canalized vessels is a feature of cellular type, while the plumped form of the endothelial cells lining belongs to the epithelioid type.1,4,5
In all types of lymph nodes hemangioma, there were no cytologic atypia, necrosis, mitoses, or extravasated erythrocytes are present. Other vascular tumors and tumourlike conditions of the lymph nodes could be a differential diagnosis of lymph node hemangiomas include lymphangioma, epithelioid vascular neoplasms, bacillary angiomatosis, the vascular transformation of the sinuses, and Kaposi's sarcoma from which it can be easily differentiated.1 Excision biopsy or surgery was curative in primary nodal hemangioma. Moreover, there were no
recurrences have been documented for nodal hemangiomas after complete excision biopsy, which is also the same result from our case. Thus, the surgeon doing tumour operation should always send the specimen to pathological examination, especially if it contains lymph node, and aware that lymph node enlargement by vascular tumor is mostly benign.
CONCLUSION
The capillary-cavernous hemangioma arising from the lymph node was an extremely rare pathological finding after oncological surgery. Treatment by surgical excision was curative. The awareness of this benign vascular tumour must be known to physicians so that it was not mistakenly diagnosed as a malignant disease with subsequent unnecessary radical therapy.
ACKNOWLEDGEMENT
None.
DISCLOSURE
The author reports no conflicts of interest in this work.
REFERENCES
-
1. Chan JK, Frizzera G, Fletcher CD, et al. Primary vascular tumors of lymph nodes other than Kaposi's sarcoma. Analysis of 39 cases and delineation of two new entities. Am J Surg Pathol. 1992;16:335-50.
-
2. Tessieras J, Chenaye J, Senechaud C, et al. Intranodal Capillary-Cavernous Hemangioma: Report of a Very Rare Case. SAGE Open Med Case Rep. 2019;7:2050313X19846710.
-
3. Sadick M, Müller-Wille R, Wildgruber M, et al. Vascular Anomalies (Part I): Classification and Diagnostics of
Vascular Anomalies. Rofo. 2018;190:825-35.
-
4. Elgoweini M, Chetty R. Primary Nodal Hemangioma. Arch Patol Lab Med. 2012;136:110-2.
-
5. Dellachà A, Fulcheri E, Campisi C. A lymph nodal capillary-cavernous
hemangioma. Lymphology. 1999;32:123-5.
-
6. Pagni F, Di Bella C. Capillary Cavernous Hemangioma of Lymph node. Int J Surg Pathol. 2010;18:338.
-
7. Reich RF, Moss S, Freedman PD. Intranodal hemangioma of the oral soft tissues: a case report of a rare entity with review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:71-3.
-
8. Goto T, Akanabe K, Maeshima A, et al. Hemangioma in a pulmonary hilar lymph node: case report. World J Surg Oncol. 2011;9:8.
-
9. Terada T. Capillary cavernous hemangioma of the lymph node. Int J Clin Exp Pathol. 2013;6:1200-1.
-
10. Müller-Wille R, Wildgruber M, Sadick M, et al. Vascular Anomalies (Part II): Interventional Therapy of Peripheral Vascular Anomalies. Rofo. 2018;190:927-37.
-
11. Wassef M, Blei F, Adams D, et al. Vascular Anomalies Classification: Recommendations From the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136:e203-
14.
25

Discussion and feedback