MULTI-INFARCT DEMENTIA
on
MULTI-INFARCT DEMENTIA
Ayu Diandra Sari1, Nyoman Ratep2, Bagus Komang Satriyasa3
1Medical student of Faculty of Medicine, Udayana University
2
2Department of Physiciatric, Faculty of Medicine Udayana University/ Sanglah General Hospital
3
3Department of Farmacology, Medical School Udayana University
ABSTRACT
Dementia is a cognitive funtional deficits thatt causes memory impairment with symptoms such as: aphasia, agnosia, apraxia or a disturbance in executive functioning (the ability to plan,sequence, and organize) that interferes with social, occupational, or interpersonal skills. Most of dementia among older people in Asia,especially Indonesia is Vascular dementia. Most of vascular dementia among older people in Indonesia is multi-infarct dementia (MID). Multi-infarct dementia (MID) is a disorder involving deterioration in mental function caused by changes or damage to the brain tissues from lack of oxygen as a result of multiple blood clots throughout the brain. Risk factor for MID include a history of: Hardening of arteries (artherosclerosis), high blood pressure (hypertension), smoking, and stroke. In MID, disruption of blood flow leads to damaged brain tissue. For diagnose the patient with MID, the most important thing we must do is anamnesis. From anamnesis, we can get history of sufficient exposure, Onset of symptoms, checking sign and doing tests, and also ask whether the patient has risks factors about MID or not. There is no known definitive treatment for MID. Treatment is based on control of symptoms. Other treatments may be advised based on the individual condition.`
Keywords: multi-infarct dementia, vascular, older adult
INTRODUCTION
Dementia is one kind of increasingly common manifested by several cognitive deficits that include memory impairment involving at least one of the following: aphasia, agnosia, apraxia or a disturbance in executive functioning (the ablity to plan,sequence, abtract, and organize) that interferes with social, occupational, or interpersonal skills.1 In the text revision of Fourth edition of Diagnostic and statistical Manual of Mental Disorders (DSM-IV-TR), dementia is “characterized by multiple cognitive defects that include impairment in memory,” without impairment in
consciousness.2 Dementia usually happen among 1%of individuals aged 60 years. The DSM-IV allow clinicians to characterize the nature of an individual’s dementia, such as Alzheimer’s type or Vascular type.1 Most of dementia among older people in Asia,especially Indonesia is Vascular dementia.3
Vascular dementia is the second most common cause of dementia in the United states and Europe in the elderly, but it is the most common form in some parts of Asia, includes Indonesia. Most of vascular dementia among older people in Indonesia is multi-infarct dementia (MID). Some research explained about 20% of all dementias are MID, affects men more often than women,over 55 years, with the onset averaging around age 65.3,4 Risk factor for MID include a history of: Hardening of arteries (artherosclerosis), high blood pressure (hypertension), smoking, and stroke.5
DEFINITION
Multi-infarct dementia (MID) is a disorder involving deterioration in mental function caused by changes or damage to the brain tissues from lack of oxygen as a result of multiple blood clots throughout the brain.6 MID usually characterized by the development multiple areas of infarction in both cortical and subcortical areas.7 Lacunar infarcts are small, punctuate lesions usually found in the deep white matter, basal ganglia, and brainstem. Multiple lacunar strokes or a few larger strokes can lead to MID.8
EPIDEMIOLOGY
Vascular dementia accounts for approximately 15% of all dementias and it is the second most common cause of dementia in the United states and Europe in the elderly, but it is
the most common parts of Asia.1,3 The 5-year survival rate is 39% for patients with vascular dementia compared with 75% for age-matched controls. Vascular dementia is associated with a higher mortality than “Alzheimer’s”, presumably because of the excess in cardiovascular risk factors. MID affects approximately 4 out to 10.000 people. It is estimated that 10 to 20% of all dementias are multi-infarct (MID and Alzheimer’s disease together account for about 30 to 60% of all dementia). MID affects both sexes but affects men more often than women.
The disorder usually affects older people, over 55 years , with the onset averaging around age 65.4 The prevalence of the illness is 1.5% in Western countries and approximately 2.2% in Japan. It accounts for 50% of all dementias in Japan, 20 to 40% in Europe and 15% in Latin America. The incidence of dementia is 9 times higher in patients who have had a stroke than in controls. 25% of stroke patients develop new-onset dementia within 1 year of their stroke. The relative risk of incident dementia is 5.5% within 4 years of suffering a stroke.4
ETIOLOGY
MID is caused by multiple strokes (disruption of blood flow to the brain).9 Risks include a history of MID, stroke, hypertension, smoking, and atherosclerosis. Atherosclerosis is associated with coronary heart disease, cerebrovascular disease, peripheral vascular disease, diabetes mellitus, and kidney disorders that require dialysis. Risks of atherosclerosis include obesity, hypertension, and high levels of blood lipids, including cholesterol and triglycerides.4 Patients with a history of hypertension and noncerebral atherosclerotic cerebrovascular disease are at increased risk for the disorder, and many patients who go on to develop vascular dementia have a previous history of
stroke. A patchy and inconsistent pattern of deficits may be seen initially, with relative
preservation of some cognitive areas. As strokes accumulate, impairment becomes more widespread and generalized in nature. A so-called stepwise course is typical, with fairly stable periods of functioning interrupted by sudden deteriorations and the establishment of a more impaired level of functioning.2
PATHOGENESIS
In MID, disruption of blood flow leads to damaged brain tissue. Some of these strokes may occur without noticeable clinical symptoms. Doctor refer to these as “silent strokes”. An individual having a silent stroke may not even know it is happening, but over time, as more areas of the brain are damaged and more small blood vessels are blocked, the symptoms of MID begin to appear.9 The disorder is associated with atherosclerosis, a condition where fatty deposits occur in the inner lining of the arteries. Atherosclerotic plaque damages the lining of an artery. Platelets clump around the area of injury (a normal part of the clotting and healing process). Cholesterol and other fats also collect at this site, forming a mass within the lining of the artery. MID is not caused directly from deposits of atherosclerotic plaque in the blood vessels of the brain, but by a series of strokes that leave areas of dead brain cells (infarction). This occurs when atherosclerotic plaques cause multiple, scattered blood clots (thrombi) that block off the small blood vessels and prevent localized areas of the brain from receiving blood flow and oxygen. The consequences vary depending on the location and severity of the infarctions. Memory impairment is often an early symptom of the disorder, followed by judgment impairment. This often progresses in a step-by-step manner to delirium, hallucinations, and impaired thinking. Personality and mood changes accompany the
deteriorating mental condition. Apathy and lack of motivation are common. Catastrophic reaction, where a person reacts to tasks by withdrawal or extreme agitation, is common. Confusion that occurs or is worsened at night is also common.4
CLINICAL FINDINGS
For diagnose the patient with MID, we must do the anamnesis. The history that we ask include History of sufficient exposure, Onset of symptoms, checking sign and doing tests, and also ask whether the patient has risks factors about MID or not. For clinical findings, we must understand about the diagnostic criteria for dementia (all types) first, so after that we can understand more about DSM-IV diagnostic criteria for vascular dementia.1
Table 1. Diagnostic criteria for dementia (all types)1
The development of multiple cognitive deficits manifested by both of the following:
-
1. Memory impairment (inability to learn new information and to recall previously learned information)
-
2. At least one of the following cognitive disturbances:
-
a. Aphasia (language disturbance)
-
b. Apraxia (inability to carry out motor activities despite intact motor function)
-
c. Agnosia (failure to recognize or identify objects despite intact sensory function) Disturbance in executive functioning (i.e, planning, organizing, sequencing, abstracting)
Table 2. DSM-IV diagnostic criteria for vascular dementia (MID)1
-
A. See Table 1.
-
B. Focal neurological signs and symptoms (eg, exaggeration of deep tendon reflexes, extensor plantar response, pseudobar palsy, gait abnormalities, weakness of an extremity) or laboratory evidence indicative of cerebrovascular disease (eg, multiple infarctions involving cortex and underlying white matter) that are judged to be etiologically related to the disturbance
-
C. The cognitive deficits cause significant impairment in social or occupational functioning and represent a significant decline from a previous level of functioning The deficits do not occur exclusively during the course of delirium.
MID also has symptoms whether help us to make diagnose easier, such as: confuse at night, decreased ability to function independently, decreased interest in daily living activities, difficulty making judgments, extreme emotional disturbance (agitation), frustation, depression, anxiety, stress, and tension from loss of mental function, inability to be spontaneous, lack of emotion, memory loss,numbness or tingling, slowly worsening memory loss (dementia), [such as confusion, disorientation, decline in many brain functions that gets worse, difficulties with attention, concentration, judgment, and behavior, difficulty thinking, false beliefs (delusions), hearing sounds or seeing things that are not there (hallucinations), personality changes, problems with language (aphasia)], swallowing difficulty, sudden involuntary laughing or crying, urinary incontinence, withdrawal from social interaction (inability to interact to social or personal situations, inability to keep a job).5
Additional symptoms that may be associated with this disease: facial paralysis, eyelid dropping, high blood pressure.
SIGN AND DIAGNOSTIC TEST
The disorder is a diagnosed based on history , symptoms, signs, and tests, and by ruling out other causes of dementia, including dementia due to metabolic causes.5 History of the dementia often shows stepwise progression of the condition: periods of abrupt decline alternating with "plateau" periods of minimal decline. Other characteristics that suggest multi-infarct dementia include: abrupt onset, somatic (physical) complaints, emotional changes, and focal (localized) neurologic signs and symptoms (modified Hachinski ischemia scale).4
Sign of MID include: abnormal reflexes, local nervous system (neurologic) signs
(on the modified Hachinski ischemia scale), past stroke or hypertension, periods of quick worsening alternating with stable periods of very little change, quick onset, weakness or loss of function on one side, one area, or many areas.
Ideally, a completed history should be obtained from someone who knows the patient well, as well as from the patient. Attention should be paid to medications, drug and alcohol use, onset and course of impairment, as well as psychosocial and medical antecedents.1
A neurologic examination shows variable deficits depending on the extent and location of damage. There may be multiple, focal neurologic deficits (localized areas with specific loss of function). Weakness or loss of function may occur on one side or only in one area. Abnormal reflexes may be present. There may be signs of cerebellar dysfunction such as loss of coordination. The following laboratory tests should be obtained as part of the dementia workup: CBC test, complete chemistry profile, urinalysis, thyroid function tests, folate and vitamin B12 levels, and syphilis serology. Additional studies are obtained based on history and examination. These may include toxicology screen, sedimentation rate, HIV and Lyme disease serology, heavy metal screen, antinuclear antibody, neuropsychological testing, chest x-ray, lumbar puncture, and neuroimaging. A chest x-ray may assist in determining the presence of pneumonia, congestive heart failure, and chronic obstructive pulmonary disease. Cerebrospinal fluid (CSF) is not routinely evaluated. A lumbar puncture may be performed for cases with unusual presentation (ie, early onset, rapid progression), suspicion of neurosyphilis, neuroborreliosis, or metastatic carcinoma. Structural neuroimaging such as CT scan or MRI cab demonstrate atrophy, white matter ischemic changes, infarcts, space occupying lesions, and normal-pressure hydrocephalus. Functional imaging such as SPECT and
PET provide information on metabolic function by measuring cerebral blood flow or
cell uptake of glucose. A commonly used cognitive screening tool is the Folstein Mini-
Mental State Examination. Patchy defects are present in persons with vascular dementia. The deficits are global in persons with Alzheimer dementia.10
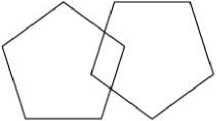
The Folstein Mini-Mental State Examination is as follows orientation: first, ask the patient the date, day, month, year, and season. The maximum score is 5. Second, ask the patient their current location, ie, facility, floor, town, state, and country. The maximum score is 5. For the registration: name 3 objects (eg, ball, flag, door), and ask the patient to repeat them. The maximum score is 3.In attention: ask the patient to spell the word "world" backwards or to subtract 7 from 100 serially backwards (stop after 5 answers). The maximum score is 5. In recall: Ask the patient to remember the 3 objects from the Registration portion of the test. The maximum score is 3. For the language: ask the patient to identify a pencil and a watch. The maximum score is 2 (Ask the patient to repeat the phrase "no ifs, ands, or buts." The maximum score is 1. Ask the patient to follow a 3-step command. The maximum score is 3. Ask the patient to read and obey the phrase "close your eyes." The maximum score is 1. Ask the patient to write a sentence. The maximum score is 1. Ask the patient to copy a set of interlocking pentagons. The maximum score is 1). The total maximum possible score is 30. Generally, any score less than 24 is considered abnormal, but the cutoff varies with the patient's level of education. Because the results for this test can vary over time, and for some people results can vary during the day, record when (ie, the time and date) this test was performed.5
The Mini-Mental State Exam
Patient___Examiner Date
Maximum Score
Orientation
5 ( ) Wι∑ιt is the (year) (season) (date) (day) (month)?
5 ( ) Where are we (state) (country) (town) (hospital) (floor)?
Registration
-
3 ( ) Name 3 objects: 1 second to say each. Then ask the patient
all 3 after you have said them. Give 1 point for each correct answer.
Then repeat them until he/she learns all 3. Count trials and record.
Trials__
Attention and Calculation
5 ( ) Serial 7's. 1 point for each correct answer. Stop after 5 answers.
Alternatively spell "world" backward.
Recall
-
3 ( ) Ask for the 3 objects repeated above. Give 1 point for each correct answer.
Language
-
2 ( ) Name a pencil and watch.
1 ( ) Repeat the following “No ifs, ands, or buts”
-
3 ( ) Follow a 3-stage command:
"Take a paper in your hand, fold it in half, and put it on the floor."
-
1 ( ) Read and obey the following: CLOSE YOUR EYES
1 ( ) Write a sentence.
1 ( ) Copy the design shown.
__ Total Score
ASSESS level of consciousness along a continuum Alert Drowsy Stupor Coma
Picture 10. The Folstein Mini-Mental State Examination5
DIFFERENTIAL DIAGNOSIS
Because of the symptoms of MID are so similar to Alzheimer’s disease, it can be difficult for a doctor to make a firm diagnosis. Since the diseases often occur together, making a single diagnosis of one or the other is even more problematic. Some research suggest that MID may cause Alzheimer’s disease or make it get worse faster. MID may be misdiagnosed as Alzheimer’s, or may be found along with Alzheimer’s.4,9
Table 3. Comparison of VaD & AD11
|
Vascular Dementia (VaD) |
Alzheimer’s Dementia(AD) | |
|
Gender |
Males more commonly |
Females commonly |
|
Genetic |
Not clear |
Suspected |
|
Onset |
Relatively sudden |
Insidious |
|
Course |
Stepwise progression |
Gradual & progress |
|
Somatic Complaints |
Common |
Rare |
|
Hypertension |
More common |
Less common |
|
Focal Neuro sign |
Present |
Unusual |
|
Personality |
Well preserved |
Disintegration |
|
Insight |
Preserved |
Lost early |
|
Affect |
Depression, Anxiety, Lability |
Affect blunted |
Beside AD, the other differential diagnosis of MID. Transcient Ischemic Attacks (TIA) are brief episodes of focal neurological dysfunction lasting less than 24 hours (usually 5 to 15 minutes). Although a variety of mechanism may be responsible, the episodes are frequently the result of microembolization from a proximal intracranial arterial lesion that produces transient brain ischemia, and the episodes usually resolve without significant pathological alteration of the parenchymal tissue. Differerentiating delirium and dementia can be more difficult than the DSM-IV classification indicates. In general, delirium is distinguished by rapid onset, brief duration, fluctuation of
cognitive impairment during the course of the day, nocturnal exacerbation of symptoms, marked disturbance of the sleep-wake cycle, and prominent in attention and perception. Some patients with depression have symptoms of cognitive impairment difficult to distinguish from symptoms of dementia. Patients with depression-related cognitive dysfunction generally have prominent depressive symptoms, have more insight into their symptoms than do demented patients, and often have a past history of depressive episodes. Persons who attempt to stimulate memory loss, as in factitious disorder, do so in an erratic and inconsistent manner. In true dementia, memory for time and place is loss before memory for person, and recent memory is lost before remote memory. Although schizophrenia may be associated with some acquired intellectual impairment, its symptoms are the related symptoms of psychosis and thought disorder seen in dementia. Aging is not necessarily associated with any significant cognitive decline but minor memory problems can occur as a normal part of aging. These normal occurrences are sometimes referred to as benign senescent forgetfullness or age-associated memory impairment. They are distinguished from dementia by their minor severity and by the fact that the do not interfere significantly with a person’s social or occupational behaviour. Mental retardation does not include memory impairment and occurs in childhood. Amnestic disorder is characterized by circumscribed loss of memory and no deterioration. Major depression in which there is impaired memory responds to antidepressant medication. Malingering and pituitary disorder must be ruled out but are unlikely.
TREATMENT
There is no known definitive treatment for MID. Treatment is based on control of symptoms. Other treatments may be advised based on the individual condition. For the initial diagnosis and treatment, the person should be in a pleasant, comfortable, non-threatening, physically safe environment for diagnosis and initial treatment. Hospitalization may be required for a short time. The underlying causes should be identified and treated as appropriate, including treatment for atherosclerosis and hypertension.
Discontinuing or changing medications that worsen confusion or that are not essential to the care of the person may improve cognitive function. Medications that may cause confusion include anticholinergics, analgesics, cimetidine, central nervous system depressants, lidocaine, and other medications. Disorders that contribute to confusion should be treated as appropriate. These may include heart failure, decreased oxygen (hypoxia), thyroid disorders, anemia, nutritional disorders, infections, and psychiatric conditions such as depression. Correction of coexisting medical and psychiatric disorders often greatly improves the mental functioning.
Medications may be required to control aggressive or agitated behaviors or behaviors that are dangerous to the person or to others. These are usually given in very low doses, with adjustment as required. Medications may include antipsychotics, beta-blockers, serotonin-affecting drugs (lithium, trazodone, buspirone, or clonazepam), fluoxetine, imipramine, or others. Sensory function should be evaluated and augmented as needed by hearing aids, glasses, or cataract surgery.
Long Term Treatment
Provision of a safe environment, control of aggressive or agitated behavior, and the ability to meet physiologic needs may require monitoring and assistance in the home or in an institutionalized setting. This may include in-home care, boarding homes, adult day care, or convalescent homes. Family counseling may help in coping with the changes required for home care. Visiting nurses or aides, volunteer services, homemakers, adult protective services, and other community resources may be helpful in caring for the person with MID. In some communities, there may be access to support groups. In any care setting, there should be familiar objects and people. Lights that are left on at night may reduce disorientation.
The schedule of activities should be simple. Behavior modification may be helpful for some persons in controlling unacceptable or dangerous behaviors. This consists of rewarding appropriate or positive behaviors and ignoring inappropriate behaviors (within the bounds of safety). Reality orientation, with repeated reinforcement of environmental and other cues, may help reduce disorientation.
Legal advice may be appropriate early in the course of the disorder. Advance directives, power of attorney, and other legal actions may make it easier to make ethical decisions regarding the care of the person with MID.4
Prevention
Control conditions that increase the risk of hardening the arteries (atherosclerosis) by: controlling high blood pressure, controlling weight, reducing saturated fats and salt in the diet, treating related disorders.
PROGNOSIS
The prognosis for individuals with MID is generally poor. The symptoms of the disorder may begin suddenly, often in a step-wise pattern after each small stroke. Some people with MID may even appear to improve for short periods of time, then decline after having more silent strokes. The disorder generally takes a downward course with intermittent periods of rapid deterioration. Death may occur from stroke, heart disease, pneumonia, or other infection.9 Possible complications that maybe happen such as: heart disease, infections anywhere in the body, loss of ability to function or care for self, loss of ability to interact, reduced lifespan, side effects of medications.5
SUMMARY
Multi-infarct dementia, also known as vascular dementia, is the second most common form of dementia after Alzheimer disease (AD) in older adults. The term refers to a group of syndromes caused by different mechanisms all resulting in vascular lesions in the brain. Early detection and accurate diagnosis are important, as vascular dementia is at least partially preventable.
Vascular dementia is the second most common cause of dementia in the United States and Europe in the elderly, but it is the most common form in some parts of Asia. The prevalence of vascular dementia is higher in men than in women and it increases with age. Vascular dementia is associated with a higher mortality than 'Alzheimer's', presumably because of the excess in cardiovascular risk factors. Risk factors for vascular dementia include hypertension, smoking, hypercholesterolemia, diabetes mellitus, and cardiovascular and cerebrovascular disease.
The recommended investigations for cognitive impairment should be carried
out, including a dementia screening blood test, chest X-Ray, CAT scan and EKG. The screening blood test should typically include full blood count, liver function tests, thyroid function tests, lipid profile, erythrocyte sedimentation rate, C reactive protein, syphilis serology, calcium serum level, fasting glucose, urea and electrolytes, vitamin B-12, folate. In selected patients HIV serology and autoantibody testing may be done.
REFERENCES
-
1. Goldman,Howard H., MD. MPH, PhD. Review of General Psychiatry. fifth edition. 2000; 189-207
-
2. Lyons, William L., MD, Yaffee, Kristine,MD. Dementia. In: Feldman, Mitchel D., MD, Mphil, Christensen, John F., PhD. Behavioral Medicine in Primary Care: A Practical Guide. Second edition. 2003; 253-262.
-
3. Wikipedia.December, 2009.Multi-infarct dementia.
-
4. Multi-infarct dementia mini information sheet.Rockville. 1999.
-
5. Luc Jasmin, MD, Ph.DMedline Plus. Multi-infarct dementia.Calfornia.2008. [citeed 2008, February, 13].
-
6. Vassilas, Christopher A. Dementia and Literature. In Advances in Psychiatric Treatment. Vol. 9. 2003; 439-445.
-
7. Lyons, William L., MD, Yaffee, Kristine,MD. Dementia. In: Feldman, Mitchel D., MD, Mphil, Christensen, John F., PhD. Behavioral Medicine in Primary Care: A Practical Guide. Second edition. 2003; 253-262.
-
8. Kentus, Joseph A., MD, Kirshner, Howard S., MD. Psychiatric Disorders in Adults: Delirium, Dementia, and Amnestic Syndromes. In: Ebert, Michael H., MD, Nurcombe, Barry, MD, Loosen, Peter T., MD, PhD, Leckman, James F., MD. Current Diagnosis & Treatment Psychiatry. Second edition. 2008; 194224.
-
9. National Institute of Neurological Disorders and Stroke. Multi-infarct dementia information page. Bethesda. 2010
-
10. Kannayiram Alagiakrishnan, MD, MBBS.Vascular dementia: eMedicine
Psychiatry.2009.
-
11. Kelompok Ilmiah AazI, Konsesus Pengenalan Dini & Penatalaksanaan
Demensia Vaskuler.2004; 1-25
17
Discussion and feedback