THE EFFECT OF SLING-BASED MANUAL THERAPY AND STABILIZATION EXERCISE FOR IMPROVING CERVICAL ALIGNMENT AND MOBILITY IN INDIVIDUAL WITH FORWARD HEAD POSTURE
on
Sport and Fitness Journal
Volume 10, No.3, September 2022: 187-196
E-ISSN: 2654-9182
THE POTENTIAL OF SLING-BASED MANUAL THERAPY AND STABILIZATION EXERCISE FOR IMPROVING CERVICAL
ALIGNMENT AND MOBILITY IN FORWARD HEAD POSTURE
I Dewa Gede Alit Kamayoga1, A A I Ayesa Febrinia Adyasputri2, I Putu Gde Surya Adhitya2, I Putu Yudi Pramana Putra2, M. Widnyana2, Anak Agung Gede Eka Septian Utama2
-
1Sports Physiology Department Medical Faculty Udayana University, Denpasar, Bali
-
2 Physiotherapy Department, Faculty of Medicine, Udayana University, Denpasar, Bali
Email: alit_kamayoga@unud.ac.id
ABSTRACT
Greater use of information and communication technologies such as computer, smartphone, or other media has a tendency to induce failure of body postures. Laptop usage has been associated with adolescent neck pain, with daily use exceeding 2-3 hours as a threshold to forward head posture. Forward head posture would reduce cervical alignment and mobility of the neck. There are exercises that intent to improve the cervical alignment and mobility, particularly sling-based manual therapy and stabilization exercises. The method in this study used a literature review or study literature articles. Searches in the selected database provided a total of 468 references, after selected 28 articles were included in this review. A sling-based manual treatment can be used to strengthen specific muscle groups by changing the sling points and heights of the dangling rope, as well as promote neuromuscular activation through dynamic contraction and stabilization exercise is to re-train global and local stability simultaneosuly through modifying motor control In summary, sling device exerts neurophysiological effects on the cervical muscle strength by activating the descending pathways, while stabilization exercises improve cervical alignment and mobility by affecting postural control through concurrent contractions of the agonist and antagonist muscles.
Key Words: Sling; Stabilization; Cervical; Forward Head Posture
INTRODUCTION
In today’s modern life, many human daily activities rely on technology-based tools to facilitate tasks that need to be done manually. Longer rest positions when using a computer, smartphone, or other media exposes individuals to greater risk factors and increase the incidence of forward head posture (FHP)1. One research determined that FHP most happens in employees, adolescents, and students2. According to the prevalence of common faulty postures among individuals, the most prevalent faulty postures were unequal shoulder degree (36%) and forward head position (25%)3. The individuals are regularly uncovered to the repetitive movements of the body that are hazardous for growing musculoskeletal symptoms. Extended use of smartphones,
=================—=———= computers, and other devices end in the adoption of static posture for an extended duration that induce neck and shoulder pain and leads to increased FHP4.
Tendency failure of body postures can appear in individuals with greater use of information and communication technologies. Laptop use has been linked to teenage neck pain, with daily computer use of more than 2-3 hours being considered as a threshold for forward head position (FHP). This change in posture can result in a spatial shift between the spine and the line of gravity, putting a strain on the connective tissues and muscles5. Numerous studies observed a relationship between forward head posture and laptop usage. Excessive anterior positioning of the top in relation to a vertical reference line is referred to as front head posture6. Changes that happen to the alignment of head and neck affect the postural defects in the sagittal plane and decrease cervical movement because of prolonged flexed head position, which impacts the balance managed by the head7. The repetitive use of smartphones, laptops, TVs, video games, or even backpacks have their own posture adapt to FHP. One of the researchers mentioned that individuals assumed increased FHP along with the length and frequency of viewing smartphone in comparison to posture neutrally. Most individuals use smartphone with a more head tilt angle and smaller neck tilt angle8.
By tightening and shortening the posterior neck muscles while weakening and extending the anterior neck muscles, forward head position can induce muscular imbalance. Forward head position decreased the cervical alignment and mobility of the neck because there is a misalignment of posture9. There are several interventions that can be used to improve the cervical alignment and mobility with FHP. To overcome the problems in FHP, interventions such as stretching, strengthening, biofeedback techniques, stabilization exercise, and manual therapy can be applied10. A few literatures states that manual therapy and stabilization exercise can improve the cervical alignment and mobility. However, it is still rare to discuss sling-based manual therapy combined with stabilization exercise. Based on this background, this study aims to examine the effect of sling-based manual therapy and stabilization exercise for improving cervical alignment and mobility in an individual with a forward head posture.
METHOD
The method in this study used a literature review or study literature articles which using secondary statistics studies end results from several numerous studies related to the effect of slingbased manual therapy and stabilization exercise on cervical alignment and mobility in individuals with forward head posture. The literature were search through an electronic database such as Pubmed, Pedro, and Google Scholar. They had been discussed approximately manual therapy, manual therapy and forward head posture, manual therapy affects craniovertebral angle with forward head posture. The studies were included in this study if they were: 1. published from 201022 , 2.in English, 2. mentioned individual and forward head posture, 3. reported about manual therapy and stabilization for forward head posture, 4. clinical trial study, experimental study, and randomized controlled trial. The studies have been excluded from this study if they were not mentioned the exercise for forward head posture.
RESULT
Searches in the selected database provided a total of 468 references. A total of 28 articles were included in this review after eliminating duplicates and checking titles, abstracts, and full text.
Records identified through database searching (n=468)
*Pubmed 273*Pedro 31*Scholar
164*
Records after duplicates removed (n=221)
Records after title & abstract
Full-text articles were eligible for inclusion (n=28)
DISCUSSION
Inappropriate Postures Lead to FHP
Individual that using computers, smartphone, and other devices are in a extra inappropriate postures than individual who are sitting upright and going through the front. Such incorrect postures might place regular stress on the neck structure, resulting in a positive FHP11. FHP is a kind of poor posture associated with increased kyphosis in the thoracic spine and anterior shoulder position12. Poor posture that has been executed in daily activities related changes within the position of the scapula when it comes to the muscle activities and phrases kinematic that therefore increase muscle strain and tension around the neck and shoulders ensuing in a variety of upper body it could be have an effect on neuromuscular symptoms13.
FHP is one of the biggest posture problems in our lives, especially for individuals depending on activities that call for long-term use of technical information in one day. Elevated FHP may be associated with neck pain due to the neck bending forward for long periods of time
and repeated movements14. Inconsistencies in the spinal cord segments can shift the load of the trunk away from the line of gravity, preventing the entire trunk from moving in a balanced manner. The increase in outward movement is the result of forward head posture that affects the alignment of other segments7.
Sling-based Manual Therapy and Stabilization Exercise
The sling-based manual treatment is separated into passive joint mobilization and segmental motor control training and is conducted in the supine position. A sling device was used for all this intervention. Passive mobilization resulted in oscillatory mobilization with a large amplitude (Maitland grade III). This approach was done three times for 60 seconds each time, with oscillations at 1 Hz and a 1-minute gap between each repetition. Segmental motor control training through repeated moves of every movement for 1 min and the therapist using the hands to assist the perfect segmental motion15. Stabilization exercise is carried out in the prone position with exercises targeting the periscapular muscle groups along with motion Y to W, L to W, and scapular retracted completed for three sets with 10-15 repetitions, chin tucks, and stretching pectoralis muscle groups16.
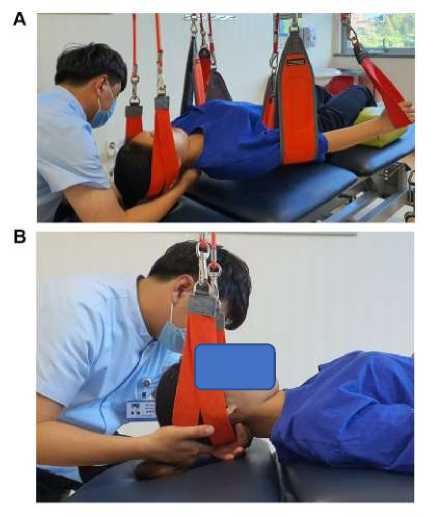
Figure. 1 Sling-Based Manual Therapy

Figure.2 Stabilization Exercises
Research has shown that sling-based manual therapy and stabilization exercises for the FHP are effective in improving cervical alignment and mobility. Sling-based manual therapy using joint mobilization is an intervention approach required to properly align the FHP14. The mobilization of the spinal joint, also known as the passive movement of the joint, is used to get the joint into the proper position with proper alignment and to increase the range of motion. Joint mobilization has the effect of inducing a reflex by stimulating articular receptors17. Meanwhile, the stabilization exercise provided stretching of the tight muscles and increasing the strength of weakened muscles so that the scapula muscles can be brought closer to the normal position18.
According to Kim (2019), manual therapy performed for 6 weeks can enhance the angle and range of motion of the craniovertebral joint. Giving this intervention include passive mobilization and segmental motor control training showed a lower in sternocleidomastoideous and anterior scalene muscle activity. Moreover, this intervention approach had a significant impact in the cervical mobility such as in flexion, extension, and rotation14. From this results it can be implied that manual therapy to direction and the level of spinal have an effect for the range of motion of the neck. Manual therapy where the loads on the neck is distinct in comparison to the load on the spine whilst it is necessary to maintain posture11. Manual therapy procedural intervention that support by applying a sling device to aims to provide the research subject in actual neutral position with optimal loading of each target segment and to make a closed kinetic chain environment for exercise. Therefore, prior to intervention, research subjects were given a sling device to allow them to move in a comfortable position only at specific spinal levels14. Due to the unstable surface, a sling-based manual treatment can be used to strengthen specific muscle groups by changing the sling points and heights of the dangling rope, as well as promote neuromuscular activation through dynamic contraction19.
Decreased the joints of neck movement and mobility was impact from forward head posture. Manual spinal treatment is effective in improving the mobility of the joints around the neck. Increased cervical range of motion was associated with a greater increase in craniovertebral angle. In addition, posterior anterior mobilization reduces cervical spine stiffness and increases
=================—=———=
range of motion. Kinetic movement of the cervical spine can be achieve with increasing the movement of the articular surface of the cervical spine, ensuing in improved angle and mobility of the craniovertebral angle20. Spinal mobilization techniques used in manual spinal treatment activate the descending pathway from the peritubular gray region (PAG) of the midbrain, reduce superficial neck flexion, and increase deep flexor activity. It has a neurophysiological effect on the strength of the neck muscles21.
Combination Sling-Based Manual Therapy and Stabilization Exercise Improving Cervical Alignment and Mobility
The occurrence of FHP can occur again in the future if when carrying out daily activities do not pay attention to the duration and position of the body when using information technology and the surrounding area when performing these activities. FHP will cause problems for other bodies if not handled properly using the proper intervention approach22. Research by Fathollahnejad et al (2019) states that giving sling-based manual therapy and stabilization exercise indicates it is more effective in improving cervical alignment and mobility in FHP16. This is also supported research by which Cho et al (2017) states manual therapy using the joint mobilization technique showed statistically and clinically significant results in craniovertebral angle, pain, cervical range motion, neck disability seen from NDI score23. The neck disability index (NDI) was used to measures neck pain and neck functional disability. This contains 10 sections including: pain intensity, personal work, lifting, studying, headache, concetration, working, driving sleeping, and recreational activities. The questionnaire is evaluated based on a likert scale from 0 (no impairment) to 5 (maximum impairment). Grade 0-4 indicate deficiency disabled, 5-15 mild disabled, 15-24 moderate disabled, 25-34 severe disabled, and over 35 complete disabled24.
Research by Fathollahnejad et al in 2019, 6 weeks and 1 month follow-up showed improved cervical spine alignment and mobility with manual therapy and stabilization exercises. This intervention approach stepped forward tissue elasticity and range of motion around the neck, alleviated it, relaxation, impaired muscle function, and reduced soft tissue swelling and inflammation16. Pain alleviation may additionaly reduce motor system depression and partially enhance function21. Some research confimed that a combination of manual therapy and stabilizing exercise become extra powerful in treating FHP than stabilizing exercise alone14,23,19.
Combined of manual therapy and stabilization exercise to overcome the problems that happens in FHP. Stabilization exercise is exercising that the usage of easy movement to enhancement the posture25. Stabilization exercises impact postural control by contracting the essential cervical stabilizer muscle at the same time as the agonist and antagonist muscles, particularly the deep neck flexor muscle26. Stabilization exercise is to re-train global and local stability simultaneosuly through modifying motor control. Activation from the local muscles, global muscles tissues that purpose to stabilizing the neck and scapula movemement act synergically to maintain normal function27. As a result, stabilization exercise improves head and neck reflex through affect the proprioception of the neck muscle groups, increasing muscle
^--=---=---=---=-=---=---=—————
contractions, and growing the environmental exposure. A better balance of muscle can be achieve from a development in proprioception28.
Research accomplished by Jaroenrungsup et al in 2021 showed that giving stabilization exercise help to correct the posture in forward head posture which can be visible on their results that there are substantial statistically in craniovertebral angle and neck disability index10. Stabilization exercise cervico-scapulothoracic strengthening and stretching can improve cervical and scapulothoracic aligment properly and prevent poor posture. The improvement of cervico-scapulothoracic alignment will affect overall muscle performance around the neck and scapula22. Stretching exercise can increase muscle flexibility and it will affect the range of motion of neck and craniovertebral angle29. FHP also provides stress to the structure and tension of the muscle tissues around the neck and stabilization exercise assist to reducing tension of muscles such as upper trapezius and Sternocleiodomastoideus so it could be relieving the muscle imbalance30.
CONCLUSION
Providing sling-based manual therapy and stabilization exercise can assist in improving the cervical alignment and mobility in adolescents with FHP. Sling-based manual therapy exerts neurophysiological effects on the cervical muscle strength by activating the descending pathways from the periaqueductal gray area (PAG) of the midbrain and the sling-based enhances neuromuscular activation through dynamic contraction due to the unstable surface as well as stabilization exercise affect the cervical alignment and mobility through concurrent contractions of the agonist and antagonist muscles, propioception of muscle, and reducint the tension of muscle around the neck. In the future, it is hoped there will be research discussing about the exercise to help overcome the problems that happen in FHP for a long-term condition.
CONFLICT OF INTEREST
The authors declare no conflict of interest
REFERENCES
-
1. Gustafsson E, Thomes S, Grimby EA, Hagberg M. Texting on mobile phones and musculoskeletal disorders in young adults: five year cohort study. Appl Ergon. 2017;58:208-214.
-
2. Kiatkulanusorn S, Suato BP, Werasirirat P. Analysis of neck and back muscle activity
during the application of various pillow designs in patients with forward head posture. J Back Musculoskelet Rehabil. 2021;34(3):431–9.
-
3. Mosaad DM, Abdel-aziem AA, Mohamed GI, Abd-Elaty EA, Mohammed KS. Effect of forward head and rounded shoulder posture on hand grip strength in asymptomatic young adults: a cross-sectional study. Bulletin of Faculty of Physical Therapy. 2020 Dec;25(1).
^--=---=---=---=-=---=---=—————
-
4. Kim DH, Kim CJ, Son SM. Neck pain in adults with forward head posture: Effects of craniovertebral angle and cervical range of motion. Osong Public Health and Research Perspectives. 2018;9(6):309–13.
-
5. Sikka I, Chawla C, Seth S, Alghadir AH, Khan M. Effects of Deep Cervical Flexor Training on Forward Head Posture, Neck Pain, and Functional Status in Adolescents Using Computer Regularly. BioMed Research International. 2020:1-7.
-
6. Lee S, Lee Y, Chung Y. Effect of changes in head postures during use of laptops on muscle activity of the neck and trunk. Physical Therapy Rehabilitation Science. 2017;6(1):33-38
-
7. Cheon S, Park S. Changes in neck and upper trunk muscle activities according to the angle of movement of the neck in subjects with forward head posture. 2017;19(2):191-193
-
8. Lee SY, Lee DH, Han SK. The effects of posture on neck flexion angle while using
a smartphone according to duration. J Korean Soc Phys Med. 2016;11(3):35-39.
-
9. Anbupriya Sureshbabu M, Nishanth H, Aishwarya A. Immediate Effect of Chin Tuck Exercises on Craniovertebral Angle and Shoulder Angle Among Collegiates with Forward Head Posture. Biomedical and Pharmacology Journal. 2021;14(4):2295–8.
-
10. Jaroenrungsup Y, Kanchanomai S, Khruakhorn S. Effects of self-posture correction exercise in forward head posture of smartphone users., Songklanakarin J. Sci. Technol. 2021: 43(2), 439-447
-
11. Alowa Z, Elsayed W. The impact of forward head posture on the electromyographic activity of the spinal muscles. J Taibah Univ Med Sci. 2021 Apr 1;16(2):224–30.
-
12. Jabbar KM, Gandomi F. The comparison of two corrective exercise approaches for hyperkyphosis and forward head posture: A quasi-experimental study. Journal of Back and Musculoskeletal Rehabilitation. 2021;34(4):677–87.
-
13. Kwon JW, Son SM, Lee K. Changes in upper-extremity muscle activities due to head position in subjects with a forward head posture and rounded shoulders. 2015; 27(6): 1739– 1742
-
14. Mingels S, Dankaerts W, van Etten L, Thijs H, Granitzer M. Comparative analysis of headtilt and forward head position during laptop use between females with postural induced headache and healthy controls. Journal of Bodywork and Movement Therapies. 2016 Jul 1;20(3):533–41.
-
15. Kim DH, Kim SY. Comparison of immediate effects of sling-based manual therapy on specific spine levels in subjects with neck pain and forward head posture: a randomized clinical trial. Disability and Rehabilitation. 2020 Sep 10;42(19):2735–42.
-
16. Fathollahnejad K, Letafatkar A, Hadadnezhad M. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: A six-week
^--=---=---=---=-=---=---=—————
intervention with a one-month follow-up study. BMC Musculoskeletal Disorders. 2019 Feb 18;20(1).
-
17. Jeon YH, Cho KH, Park SJ. Effects of neuromuscular electrical stimulation (NMES) plus upper cervical spine mobilization on forward head posture and swallowing function in stroke patients with dysphagia. Brain Sciences. 2020 Aug 1;10(8):1–10.
-
18. Kang JI, Choi HH, Jeong DK, Choi H, Moon YJ, Park JS. Effect of scapular stabilization exercise on neck alignment and muscle activity in patients with forward head posture. 2018; 30(6): 804–808.
-
19. Kim SY, An CM, Cha YS, Kim DH. Effects of sling-based manual therapy on cervicothoracic junction in patients with neck pain and forward head posture: A randomized clinical trial. Journal of Bodywork and Movement Therapies. 2021 Jul 1;27:447–54.
-
20. Ghan GM, Babu VS. Immediate Effect of Cervico-thoracic Mobilization on Deep Neck Flexors Strength in Individuals with Forward Head Posture: A Randomized Controlled Trial. Journal of Manual and Manipulative Therapy. 2021;29(3):147–57.
-
21. An HJ, Park SJ. Effects of Cervical Spine Mobilization on Respiratory Function and Cervical Angles of Stroke Patients: A Pilot Study. 2021;9(4):1-9
-
22. Mahmoud NF, Hassan KA, Abdelmajeed SF, Moustafa IM, Silva AG. The Relationship Between Forward Head Posture and Neck Pain: a Systematic Review and Meta-Analysis. Vol. 12, Current Reviews in Musculoskeletal Medicine. Springer; 2019. p. 562–77.
-
23. Cho J, Lee E, Lee S. Upper thoracic spine mobilization and mobility exercise versus upper cervical spine mobilization and stabilization exercise in individuals with forward head posture: A randomized clinical trial. BMC Musculoskeletal Disorders. 2017 Dec 12;18(1).
-
24. Raoofi, Z, Sarrafzadeh J, Emrani S, Ghorbanpour A. Relationship between forward head posture and neck pain as well as disability. Journal of Clinical Physiotherapy Research. 2019;4(1):26-30.
-
25. Thigpen CA, Lynch SS, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. British Journal of Sports Medicine. 2010 Apr;44(5):376–81.
-
26. Im B, Kim young, Chung Ijung, Hwang S. Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. 2016;28(3):951-955
-
27. Irani S, Abbaszadeh-Amirdehi M, Hosseini SR, Sum S, Matlabi H, Mirasi S. The Effect of Head and Neck Stabilization Exercises on Dynamic Balance in the Elderly with Forward Head Posture. Journal of Modern Rehabilitation. 2022;16(1):9-15.
-
28. Salehi S, Hedayati R, Bakhtiari AH, sanjari M ali, Ghorbani R. The Comparative Study of the Effect of Stabilization Exercise and Stretching-Strengthening Exercise on Balance
Parameters in Forward Head Posture Patients. Archives of Rehabilitation [Internet]. 2013 [cited 2022 May 12];14(1):50–60.
-
29. Ruivo RM, Carita AI, Pezarat-Correia P. The effects of training and detraining after an 8 month resistance and stretching training program on forward head and protracted shoulder postures in adolescents: Randomised controlled study. Manual Therapy. 2016 Feb 1;21:76– 82.
-
30. Shiravi S, Letafatkar A, Bertozzi L, Pillastrini P, Khaleghi Tazji M. Efficacy of Abdominal Control Feedback and Scapula Stabilization Exercises in Participants with Forward Head, Round Shoulder Postures and Neck Movement Impairment. Sports Health. 2019 May 1;11(3):272–9.
196
Discussion and feedback