THE EFFECT OF RESISTANCE TRAINING ON TRABECULAR BONE SCORE
on
Sport and Fitness Journal
Volume 11, No.2, May 2023: 153-160
E-ISSN: 2654-9182
THE EFFECT OF RESISTANCE TRAINING ON TRABECULAR BONE SCORE
Lia Wijaya1*, Clarin Hayes1, Indira Juhanna2, Adiartha Griadhi 2
-
1 Anti Aging Medicine Magister Program, Faculty of Medicine Universitas Udayana, 80234, Denpasar, Indonesia
-
2 Physiology Department Faculty of Medicine Universitas Udayana, 80234, Denpasar, Indonesia Email : liawijaya.dr@gmail.com
ABSTRACT
Bone density is a crucial parameter for assessing healthy bones across various demographics. It is widely known that bone density decreases with age. However, surprising findings indicate that not only older individuals but also young female athletes, overweight women, adults, and even children exhibit low bone density, increasing the risk of osteoporosis and fractures. While bone mineral density (BMD) is commonly used to evaluate bone quality and diagnose osteoporosis, trabecular bone score (TBS) is considered a superior measure for assessing bone quality. Unfortunately, limited research has focused on TBS, with most studies relying on BMD as the primary parameter. This literature review aims to provide data on the effects of resistance training on TBS, aiming to improve early prediction and prevention of morbidity and mortality associated with osteoporosis-related fractures. The review includes articles published in the last decade in English, specifically discussing resistance training and TBS. Five studies were analyzed, including three experimental studies and two case-control studies. The results suggest that resistance training stimulates bone gain, as evidenced by increased TBS values in the resistance training groups compared to control or other sport groups. This holds significant potential in preventing future morbidity such as osteoporotic fractures and promoting overall well-being.
Keywords: trabecular bone score; resistance training; osteoporosis
INTRODUCTION
Healthy bones are characterized with strong and dense bones. These characteristics vary across sex and age.1 Physiologically, as we age, bone strength and density decrease, leading to increased risk of pathological fracture that affects the quality of life and independence.2 This is one of bone aging process. Surprisingly, not only aged population, young female athletes, young overweight women, adults, and even children are also possible to have low bone density.3–7 Thus, the authors think it is very important to assess one’s bone quality early on and find the right method to be able to prevent bone density related disease that enhances the quality of life.
As we age, we can get a considerable amount of bone loss if not accompanied by proper exercise.8 Exercise, specifically resistance training (RT), has been known as the best non pharmacologic treatment to rise bone density.9 RT can stimulate and maintain bone gain.10,11 This type of exercise induces tensional stimuli to the bones, which increase the bone mineral content through producing mechanical modulation of the osteogenic response.12 It has also been shown that long-term RT protocols have demonstrated to improve bone mineral density of the spine, hip, as well as the upper limbs, up to 3.8% from baseline.9,12 It has been proven that resistance training is more superior in elevating bone health than non-weight-bearing exercise. 13–15
Bone quality is usually assessed by the parameter of bone mineral density (BMD), which is the golden standard for diagnosing osteoporosis. But studies prove that trabecular bone score (TBS) is more superior in predicting risk fracture independently compared to BMD; as the prediction value from BMD overlaps up to 45% for those elderly that does not have a fracture.16 TBS captures information relating to trabecular microarchitecture.17 A bone microarchitecture study done by Shanbhogue et al. found that that suffer more bone loss compared to men with aging, whereas most of it comes from cortical bone loss at the periphery. This explains as to why osteoporosis-related-fractures happen more in elderly woman and for the most of it occur on the cortical peripheral site 1 Another conventional assessment to predict osteoporotic fracture risk is the fracture risk assessment tool (FRAX) score, which predicts the 10-year risk of major osteoporotic fracture in patients. FRAX score can also be adjusted to TBS to produce far more accurate scoring. TBS gives great clinical relevance and does not need additional high cost as it can be assessed together with BMD on a dual X-ray absorptiometry (DXA) machine.16 Unfortunately there were not many studies available on this topic since most of the studies are using BMD as its bone quality parameter. This literature review is made to give data about the effect of RT on TBS for better early prediction and prevent further morbidity and possible mortality caused by osteoporosis-related fractures.
METHODS
We searched for studies on multiple journal databases like Google Scholar, ScienceDirect, PubMed and MEDLINE because those sites provide a big bibliographic database of scientific and medical publications from well-reputed publishers. The inclusion criteria are published in English, discussing resistance training and bone trabecular score, and published in the last 10 years (2014-2023) for relevance. The keywords that were used are “ resistance training OR strength training AND TBS OR trabecular bone
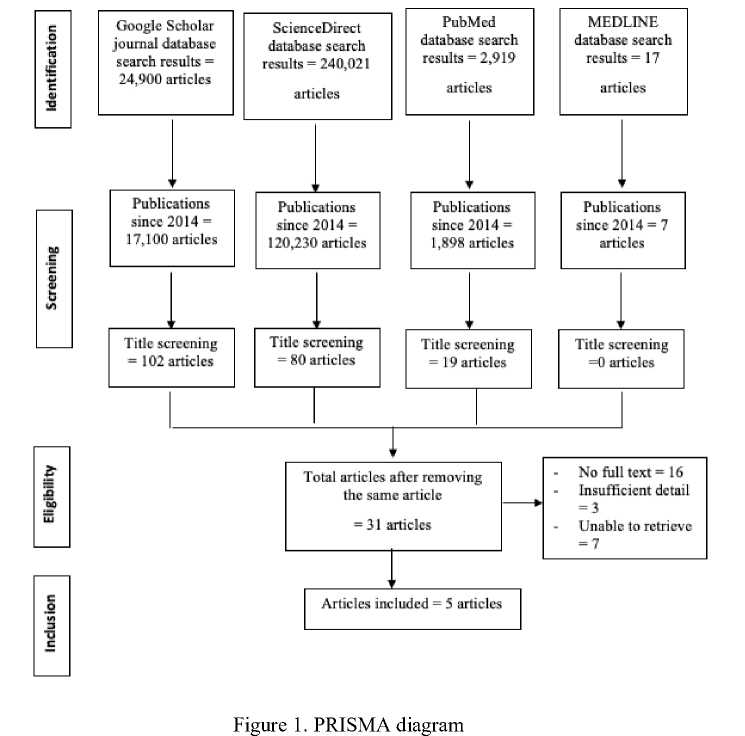
Writers use these search keywords across these platforms Google Scholar, ScienceDirect, PubMed and MEDLINE. Search results are 24,900, 240,021, 2,919, and 17 studies respectively. Writers then filter out studies done before 2014 resulting 17,100, 120,230, 1,898, and 7 studies left respectively. Writers then do title screening, most of the articles doesn’t explain resistance training and TBS, yet the keywords are found in the bibliography. Some other articles only mention those keywords yet the articles doesn’t use TBS as their study parameter. Thus resulting only 102, 80, 19, and 0 articles left respectively. Writers then remove same articles resulting 31 articles left. No full text was found on 16 articles, 3 articles have no sufficient details, and 7 articles are unable to retrieve. There was a total of 5 studies (3 experimental studies and 2 case-control studies) that fulfilled the criteria.
RESULTS
Table 1. Effects of resistance training on various studies
|
Authors |
Design |
Subjects |
Interventions |
Results |
|
El Khoury et al. 18 |
Experimental |
13 overweight young men, 18-30 years old |
The subjects trained three times per week for one year Training sessions included muscle-strengthening programs at a load that is equal to 75 percent of maximum strength. |
TBS increased significantly. |
|
Berro et al. 19 |
Experimental |
43 overweight women, 18-35 years old |
Participants were randomly allocated into three groups. The first group (15 individuals) underwent resistance training (RTG). The second group (14 individuals) underwent endurance training (ETG) The third group (14 individuals) was the control group (CG). The three groups were maintained for a period of 12 months. |
The first group (RTG) exhibited noteworthy enhancements in several areas such as lean mass, maximal strength, maximal aerobic velocity, TBS, strength index, compression strength index, bending strength index, and impact strength index. |
|
Daly et al. 14 |
Cross- |
88 female athletes |
The athletes were put into |
The athletes who |
|
sectional |
from Finland and 19 habitually active women, 17 40 years old |
five groups based on their sport-specific training history: high-magnitude (powerlifters), repetitive impact (endurance runners), repetitive nonimpact (swimmers), oddimpact (soccer players and squash players), and high-impact (triple jumpers and high jumpers). TBS values were determined from lumbar vertebral L1-L4 DXA images while also measuring body weight, height, fat-%, lean mass, isometric maximal leg press force, dynamic peak |
were subjected to intense axial loading (powerlifters with high-magnitude loading) had slightly higher TBS values compared to the reference group. |
|
jumping force, and lumbar | ||||
|
Pinho et al. 20 |
Experimental |
38 sedentary |
BMD. Subjects were randomly assigned to an experimental group (21 participants) or a control group (17 participants). The experimental group participated in thrice-weekly 60-minute sessions of power training and high-impact exercises for 20 weeks on non-consecutive days. Subjects were randomly |
Lumbar spine TBS |
|
Seaton et al. 21 |
Cross- |
elderly women, 60-70 years old 104 women and 37 |
allocated into experimental (thrice-weekly 60-minute sessions of power training and high-impact exercises for 20 weeks on non-consecutive days) (N = 21) and a control group (N = 17) The study measured several |
increased significantly. Upper body strength |
|
sectional |
men, 72.5±5.1 years old |
factors in all participants, including lumbar spine TBS (L1-L4) and bone density using DXA, along with total body and trunk lean mass. Additionally, upper and lower body strength was assessed through 1-RM tests for the seated row and leg press exercises, respectively. Hand grip strength and usual walking speed were also measured. |
(seated row with 1-RM test) significantly predicted TBS. | |
TBS: Trabecular Bone Score, 1-RM test: 1-repetition maximum test (the maximal weight an individual can lift for only one repetition with correct technique)
DISCUSSION
DXA machine has been widely used to assess BMD, the gold standard for osteoporosis diagnosis. BMD measures the amount of minerals present in the segment of bone tissue. To diagnose or manage osteoporosis, BMD values are measured in specific regions of interest within the images, typically expressed in grams per square meter (g/m2). The regions of interest commonly evaluated include the lumbar spine (LS), femoral neck, total hip, and/or 1/3 radius. BMD has few drawbacks which people with type 2 diabetes tend to have normal or higher BMD levels compared to non-diabetic patients because of the anabolic effect of the insulin. LS BMD also is usually overestimated if degenerative changes in the spine or aortic calcification are present. DXA workup is simple, easy, quick, painless and safe because it uses a low dose of dual x-rays compared to x-ray or CT-scan. As the technology progresses, it enables DXA to assess other bone health parameters besides BMD. It improves the spatial resolution thus vertebral fractures are easier to find and the assessment of TBS. 16
TBS is a method of assessing the microarchitecture of vertebral bones through the analysis of texture from spine DXA scans. It can predict the risk of fractures independently of BMD. The bone turnover process is generally balanced in healthy young adults, where the bone formation rate is equivalent to the
rate of bone resorption. However, certain factors such as chronic illness, aging, and exposure to glucocorticoids can accelerate the bone remodeling process, leading to a decline in mineralized bone over time. When bone turnover speeds up, it can affect trabecular and cortical bone differently. Trabecular bone, with a higher surface area to mass ratio, can be depleted faster than cortical bone. During each remodeling cycle, there is an overall bone tissue loss. When there is a deficiency of estrogen, for instance, bone remodeling rates may increase, resulting in the initial loss of bone in skeletal sites with high trabecular bone levels such as the spine. Later on, locations with a combination of trabecular and cortical bone, like the hip, may show visible bone loss.10 This may explain why TBS is more accurate in predicting risk fracture compared to BMD. TBS analyzes bone texture by evaluating the variations in gray levels of pixels in DXA images of the lumbar spine that have already been obtained through computer processing. TBS is a measure of bone microarchitecture derived from analyzing the texture of DXA scans of the spine. High TBS values indicate a strong bone with a microarchitecture resistant to fractures, while low TBS values indicate a weak and prone-to-fracture microarchitecture. TBS can differentiate between two 3D microarchitectures with the same bone density based on differences in trabecular characteristics.16 To obtain TBS, DXA images of the AP lumbar spine are re-analyzed, allowing for direct comparison with areal BMD and application to existing datasets.17 However, caution is required when interpreting TBS measurements since they are based on lumbar spine DXA scans, which can be affected by degenerative changes in overall body composition and the spine.22
Evidence has indicated that exercise, particularly resistance training, can have positive effects on bone metabolism. Resistance training involves moving joints against resistance, which can be achieved through various means such as weights, machines, or one's own body weight. 23 Resistance training may be an effective non-pharmacological strategy for improving bone mineral density, particularly in the treatment of age-related osteoporosis.24 Previous studies have shown that untrained or sedentary individuals who participate in resistance training for 6-12 months can experience an increase in trabecular bone architecture without increasing the reabsorption index.23 We can see from the result section, studies done by Pinho et al.20, El Khoury et al.18, Berro et al.19, and Daly et al.14 all found that resistance training groups has better TBS value compared to control groups or other exercise groups. This may be explained by Frost's mechanostat theory. It suggests that high strain produced during exercise can greatly improve the mechanical properties of bone. That is why in the study done by Daly et al.,14 swimmer group didn’t elicit enough TBS value rise because swimming is a low impact exercise. However, the bone response to resistance exercise is often site-specific, meaning that only the trained site will experience an increase in bone mineral density.24
RT has been studied extensively due to the indirect mechanical stimulus it provides to bones through joint reaction force and muscle strengthening.23 We can also see this correlation on the study result done by Berro et al.19 whereas TBS enhancement were accompanied with enhancement on maximal strength, strength index, compression strength index, bending strength index, and impact strength index. This is also in line with the study conducted by Seaton et al.21, where TBS can be predicted with upper body strength.
RT has several advantages, including enhancing individual performance such as boosting the performance of motor skills, gaining power and speed, building physical literacy, and reducing injury risk along with facilitating injury rehabilitation. It also has health benefits like boosting muscular strength, power, and local muscular endurance, enhancing cardiovascular fitness, and improving body composition. Furthermore, it has musculoskeletal benefits like enhancing BMD, insulin sensitivity, blood lipid profiles, improving resistance to injury, and promoting mental health.25
Factors that affect bone indexes, such as TBS or BMD, include serum vitamin D, pro-oxidantoxidant balance, and physical activity level, so it's important to follow a diet with enough calcium, and if dietary intake is insufficient, consider taking calcium supplements (1200 mg/day for women ≥51 years and men ≥71 years, 1000 mg/day for men aged 50-70 years). It's also recommended to monitor levels of 25-hydroxyvitamin D in the blood and ensure that they are sufficient, which may require taking vitamin D supplements (800-1000 units/day). If one’s having malabsorption then a serum 25(OH) vitamin D level of ≥30 ng/mL is advised for those with known or suspected metabolic bone disease. Exercise
recommendations include weightlifting exercises with proper posture and technique, use of elastic exercise bands for pulling movements, safe use of weight machines, lifting one's body weight through exercises like toe rises and one-foot stands, balance exercises that train the legs and challenge balance, such as controlled dancing or tai chi, more complex balance exercises that involve cognitive elements, like walking a pattern while holding a cup, posture exercises that strengthen the muscles in the back and promote core stability, and functional exercises that simulate daily movements and activities. 26 10
The limitation of this study is that previous original articles regarding RT and TBS are still limited (even though TBS gives great clinical relevance with no significant additional cost) and unspecified, the subjects of previous studies were too varied in range from age, occupation, activity level, sex. Therefore it has been challenging to find specific population of the study.
CONCLUSION
The studies mentioned in result indicate that RT can have a positive impact on bone microstructure, as it exerts mechanical stress on the bones, leading to an increase in their strength. The study suggests that RT is crucial for maintaining musculoskeletal health and is an effective strategy for improving and preserving bone quality in both younger and older populations. Based on this information, RT is considered the most effective approach to enhancing bone health. Although several studies about resistance training’s effect on trabecular bone score have already been gathered and proposed, comprehensive reviews are still limited as the population is very varied. It would also be helpful if further studies can explain the physiology mechanism of resistance training in the trabecular bone score. We would also suggest evaluating bone quality not only from BMD as the gold standard of osteoporosis, but also analysing a few more comprehensive parameters like TBS with clinical factors that are taken into account in managing osteoporosis and fracture risk management.
CONFLICT OF INTEREST
The conflicting interests of the authors are non-existent.
REFERENCES
-
1. Shanbhogue V V., Brixen K, Hansen S. Age- and Sex-Related Changes in Bone Microarchitecture and
Estimated Strength: A Three-Year Prospective Study Using HRpQCT. J Bone Miner Res [Internet]. 2016 Aug 1 [cited 2023 Jun 16];31(8):1541–9. Available from:
https://onlinelibrary.wiley.com/doi/full/10.1002/jbmr.2817
-
2. Goltzman D. The Aging Skeleton. Adv Exp Med Biol [Internet]. 2019 [cited 2023 Jun 16];1164:153–60.
Available from: https://pubmed.ncbi.nlm.nih.gov/31576547/
-
3. Bachrach LK, Gordon CM, Sills IN, Lynch JL, Casella SJ, DiMeglio LA, et al. Bone Densitometry in Children
and Adolescents. Pediatrics [Internet]. 2016 Oct 1;138(4). Available from:
-
4. MacKnight JM. Osteopenia and Osteoporosis in Female Athletes. Clin Sports Med [Internet]. 2017
Oct;36(4):687–702. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0278591917300534
-
5. Rokoff LB, Rifas-Shiman SL, Switkowski KM, Young JG, Rosen CJ, Oken E, et al. Body composition and
bone mineral density in childhood. Bone [Internet]. 2019 Apr 1 [cited 2023 Jun 16];121:9–15. Available from: https://pubmed.ncbi.nlm.nih.gov/30557635/
-
6. Hou J, He C, He W, Yang M, Luo X, Li C. Obesity and Bone Health: A Complex Link. Front Cell Dev Biol
[Internet]. 2020 Dec 21 [cited 2023 Jun 16];8. Available from: /pmc/articles/PMC7779553/
-
7. Hammoud E, Toumi H, Jacob C, Pinti A, Lespessailles E, El Hage R. Does the Severity of Obesity Influence
Bone Mineral Density Values in Premenopausal Women? J Clin Densitom [Internet]. 2021 Apr;24(2):225–
-
32. Available from: https://linkinghub.elsevier.com/retrieve/pii/S109469501930054X
-
8. Salari N, Ghasemi H, Mohammadi L, Behzadi M hasan, Rabieenia E, Shohaimi S, et al. The global prevalence
of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res [Internet]. 2021 Dec 1 [cited 2023 Apr 23];16(1):1–20. Available from: https://josr-
online.biomedcentral.com/articles/10.1186/s13018-021-02772-0
-
9. Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR. High-Intensity Resistance and Impact
Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women With Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trial. J Bone Miner Res [Internet]. 2018 Feb 1 [cited 2023 Jun 16];33(2):211–20. Available from:
https://onlinelibrary.wiley.com/doi/full/10.1002/jbmr.3284
-
10. LeBoff MS, Greenspan SL, Insogna KL, Lewiecki EM, Saag KG, Singer AJ, et al. The clinician’s guide to
prevention and treatment of osteoporosis. Osteoporos Int. 2022;33(10):2049–102.
-
11. Iwamoto J. [A role of exercise and sports in the prevention of osteoporosis.]. Clin Calcium [Internet]. 2017
Jan 1 [cited 2023 Apr 23];27(1):17–23. Available from: https://europepmc.org/article/med/28017941
-
12. Massini DA, Nedog FH, de Oliveira TP, Almeida TAF, Santana CAA, Neiva CM, et al. The Effect of
Resistance Training on Bone Mineral Density in Older Adults: A Systematic Review and Meta-Analysis. Healthc [Internet]. 2022 Jun 1 [cited 2023 Jun 16];10(6):1129. Available from: https://www.mdpi.com/2227-9032/10/6/1129/htm
-
13. Nasr R, Al Rassy N, Watelain E, Ishac S, Abdul Al O, El Hage R. Influence of three different types of physical
training programs on bone mineral density in a group of elderly subjects. Sci Sports. 2019 Jun 1;34(3):186– 9.
-
14. Daly RM, Dalla Via J, Fyfe JJ, Nikander R, Kukuljan S. Effects of exercise frequency and training volume on
bone changes following a multi-component exercise intervention in middle aged and older men: Secondary analysis of an 18-month randomized controlled trial. Bone. 2021 Jul 1;148:115944.
-
15. Shanb AA, Youssef EF. The impact of adding weight-bearing exercise versus nonweight bearing programs to
the medical treatment of elderly patients with osteoporosis. J Family Community Med [Internet]. 2014 Dec 1 [cited 2023 Apr 23];21(3):176. Available from: /pmc/articles/PMC4214007/
-
16. Shevroja E, Cafarelli FP, Guglielmi G, Hans D. DXA parameters, Trabecular Bone Score (TBS) and Bone
Mineral Density (BMD), in fracture risk prediction in endocrine-mediated secondary osteoporosis. Endocrine [Internet]. 2021;74(1):20–8. Available from: http://dx.doi.org/10.1007/s12020-021-02806-x
-
17. Harvey NC, Glüer CC, Binkley N, McCloskey E V., Brandi ML, Cooper C, et al. Trabecular bone score (TBS)
as a new complementary approach for osteoporosis evaluation in clinical practice. Bone. 2015 Sep 1;78:216– 24.
-
18. El Khoury C, Lespessailles E, Pinti A, Maalouf G, Matta J, Frenn F, et al. Effets d’un an d’entrainement de
force sur les paramètres osseux chez des jeunes hommes en surcharge pondérale. Rev Rhum. 2016 Nov 1;83:A297.
-
19. Berro AJ, Kazwini S, Ahmaidi S, El Hage R. Effects of 12 months of resistance training vs. endurance training
on bone mineral density, hip geometry indices and trabecular bone score in a group of young overweight women. Sci Sports. 2020 Oct 1;35(5):318–9.
-
20. Pinho JP, Amadio AC, Forner-Cordero A, Rodrigues Pereira RM, Hernandez AJ, Dorea EL, et al. A High-
Intensity Exercise Intervention Improves Older Women Lumbar Spine and Distal Tibia Bone Microstructure and Function: A 20-Week Randomized Controlled Trial. IEEE J Transl Eng Heal Med [Internet]. 2020 [cited 2023 Apr 18];8. Available from: /pmc/articles/PMC6964965/
-
21. Seaton MP, Nichols JF, Rauh MJ, Kado DM, Wetherell JL, Lenze EJ, et al. Associations of Lean Mass,
Muscular Strength, and Physical Function with Trabecular Bone Score in Older Adults. J Clin Densitom [Internet]. 2023 Apr 12 [cited 2023 Apr 18];101370. Available from:
https://linkinghub.elsevier.com/retrieve/pii/S1094695023000203
-
22. Cauley JA, Nelson DA. Race, ethnicity, and osteoporosis. Marcus Feldman’s Osteoporos. 2021 Jan 1;453–
75.
-
23. Benedetti MG, Furlini G, Zati A, Mauro GL. The Effectiveness of Physical Exercise on Bone Density in
Osteoporotic Patients. Biomed Res Int [Internet]. 2018 [cited 2023 Apr 29];2018. Available from: /pmc/articles/PMC6323511/
-
24. Zhao R, Zhao M, Xu Z. The effects of differing resistance training modes on the preservation of bone mineral
density in postmenopausal women: a meta-analysis. Osteoporos Int [Internet]. 2015 May 1 [cited 2023 Apr 28];26(5):1605–18. Available from: https://pubmed.ncbi.nlm.nih.gov/25603795/
-
25. Stricker PR, Faigenbaum AD, McCambridge TM. Resistance training for children and adolescents. Pediatrics
[Internet]. 2020 Jun 1 [cited 2023 Apr 28];145(6). Available from:
/pediatrics/article/145/6/e20201011/76942/Resistance-Training-for-Children-and-Adolescents
-
26. Moafian F, Sharifan P, Assaran Darban R, Khorasanchi Z, Amiri Z, Roohi S, et al. Factors Associated With
Trabecular Bone Score and Bone Mineral Density; A Machine Learning Approach. J Clin Densitom. 2022 Oct 1;25(4):518–27.
160
Discussion and feedback