ANTIBIOTICS USAGE OVERVIEW IN ORTHOPEDIC SURGERY PATIENTS AT A HOSPITAL IN BALI
on

Journal Pharmaceutical Science and Application Volume 4, Issue 2, Page 76-81, December 2022 E-ISSN: 2301-7708
ANTIBIOTICS USAGE OVERVIEW IN ORTHOPEDIC SURGERY PATIENTS AT A HOSPITAL IN BALI
Putu Ary Pudak Wangi1, Made Krisna Adi Jaya1*
1Departement of Pharmacy, Faculty of Math and Sciences, Udayana University
Corresponding author email: krisnaadijaya@unud.ac.id*
ABSTRACT
Backgrounds: Antibiotic resistance can be prevented by controlling the use of antibiotics wisely. Based on WHO recommendations, controlling the use of antibiotics is done by grouping antibiotics with the AWaRe category. Objective: This work aims to present an overview of the use of antibiotics in orthopaedic surgery patients as an effort to monitor the use of antibiotics in a hospital in Bali. Methods: Based on the patient's medical record data, the antibiotics used for orthopaedic surgery were calculated and grouped with the AWaRe classification. Result: Results showed that the most prescribed antibiotic was ceftriaxone (84.74%). There were no antibiotics in the reserve category, but the highest percentage was 94.92% in the watch category, and the access category was 5.08%. Conclusion: There is still non-selective use of antibiotics in this hospital, so in the future, it is necessary to evaluate qualitatively and quantitatively to ensure rational use as well as efforts to prevent the occurrence of antibiotic resistance.
Keywords: Antibiotics; Resistance; AwaRe; Hospital; Bali
INTRODUCTION
Antibiotic resistance is a major threat in the world of health. Antibiotic resistance occurs when the effectiveness of an antibiotic is reduced due to mutations in the infectious bacteria. National antimicrobial resistance survey data from the Indonesian Ministry of Health shows that the prevalence of multidrug resistant organisms (MDRO) ranges from 50%-82%. The Global
Antimicrobial Surveillance System (GLASS) research results in 2019 stated that there was an increase in the percentage of antimicrobial resistance in Indonesia, including carbapenems, fluoroquinolones, and third-generation cephalosporins[1]. Research by Waridiarto et al. (2015)[2] at dr. Kariadi Hospital shows that 53.3% of the use of antibiotics was irrational in cases of orthopaedic surgery.
Antibiotic resistance can be prevented through the wise use of
antibiotics. Wise use of antibiotics is the rational use of antibiotics by considering the impact of the emergence and spread of resistant bacteria. The application of wise use of antibiotics is known as 'Antibiotic Stewardship' which aims to improve patient outcomes in a coordinated manner through improving the quality of antibiotic use, which includes making a diagnosis, choosing the right type of antibiotic, dose, interval, route, and duration of administration[3].
Based on WHO recommendations (2019), controlling the use of antibiotics can be done by grouping antibiotics in the AWaRe category: Access, Watch, and Reserve. 'Access' antibiotics are the first or second-line treatment for common infections. Antibiotics of this group should be widely accessible. Antibiotics in the 'Watch' category should be applied only to a limited group of well-defined syndromes. Their use must be closely
Wangi and Jaya monitored. Antibiotics in the 'Reserve' group are treated as a last resort for the treatment of confirmed or suspected bacterial infections due to multi-drug resistant bacteria (multi-drug resistant bacteria or extensively-drug resistant bacteria) or when all alternatives fail or are not suitable[4].
This categorization supports WHO's global action plan for controlling antimicrobial resistance. This grouping aims to facilitate the application of antibiotic stewardship at the local, national and global levels; improve treatment results; suppress the emergence of resistant bacteria, and maintain the long-term benefits of antibiotics[3]. Third-generation cephalosporin antibiotics, such as ceftriaxone, cefixime, and cefoperazone, often used in orthopedic surgery cases, are included in the watch group and have high resistance potential. If there is still free use of these types of antibiotics, it is necessary to study and evaluate their use to prevent the occurrence of antibiotic resistance. Research related to the description of the use of antibiotics in orthopaedic surgery patients based on the AWaRe classification in hospitals in Bali has never been done, so it is important to carry out this as an effort to monitor the use of antibiotics.
METHODS
This research is a retrospective study of orthopaedic surgery patients receiving antibiotics. This research was conducted in the medical records department at one of the government hospitals in Bali, Indonesia, from September to December 2022. The research was declared ethically feasible and obtained ethical clearance under number
2912/UN14.2.2.VII.14/LT/2022.
The sample in this study is medical records of adult orthopaedic surgery patients aged 18-59 years who were hospitalized and received antibiotics at a hospital in Bali from January to August
2022. Data used in this study is complete patient medical record data, including medical record number, patient's age, sex, weight, height, medical history, and type of antibiotic. Data obtained were recorded on a data collection sheet and then presented descriptively, including patient socio-demographic data and patterns of antibiotic use. The types of antibiotics used were then grouped based on the AWaRe classification.
RESULTS
The data studied were 45 medical records of adult patients with orthopaedic surgery cases. Patient demographics can be seen in Table 1.
Table 1. Sociodemography of Adult Orthopedic Surgery Patients
Characteristics Amount Percentage (%)
|
Age Group | ||
|
18-24 years |
13 |
28.89 |
|
25-31 years |
8 |
17.78 |
|
32-38 years |
4 |
8.89 |
|
39-45 years |
8 |
17.78 |
|
46-52 years |
4 |
8.89 |
|
53-59 years |
8 |
17.78 |
|
Total |
45 |
100 |
|
Gender | ||
|
Man |
29 |
64.44 |
|
Woman |
16 |
35.56 |
|
Total |
45 |
100 |
|
Disease History | ||
|
No History |
43 |
95.56 |
|
Hypertension |
1 |
2.22 |
|
Pneumonia |
1 |
2.22 |
|
Total |
45 |
100 |
During the period from January to August 2022, 5 types of antibiotics were prescribed to 45 orthopaedic surgery patients. Those are ceftriaxone, cefazoline, cefoperazone, gentamicin, and cefixime, with a total of 118 antibiotic prescriptions. There were ten patients who used two types of antibiotics during hospitalization. Observational data on the pattern of prescribing types of antibiotics can be seen in Table 2.
Table 2. Use of Antibiotics in Adult Hospitalized Patients with Orthopedic Surgery
|
Type of antibiotic |
AWaRe Classification (WHO, 2019) |
Dosage (gram) |
Number of prescriptions |
Percentage of prescriptions (%) |
Percentage according to AWaRe classification (%) |
|
1 |
53 |
53 | |||
|
Ceftriaxone |
Watch |
2 |
47 |
47 | |
|
Total |
100 |
84.74 | |||
|
1 |
2 |
66,67 | |||
|
Cefoporazone |
Watch |
2 |
1 |
33.33 |
94.92 |
|
Total |
3 |
2.54 | |||
|
0.1 |
1 |
11.11 | |||
|
Cefixime |
Watch |
0.2 |
8 |
88.89 | |
|
Total |
9 |
7.62 | |||
|
0.04 |
2 |
50 | |||
|
Gentamicin |
Access |
0.08 |
2 |
50 |
5.08 |
|
Total |
4 |
3.38 | |||
|
Cefazoline |
Access |
1 |
2 |
1.69 | |
|
Total Prescriptions |
118 |
100 |
100 | ||
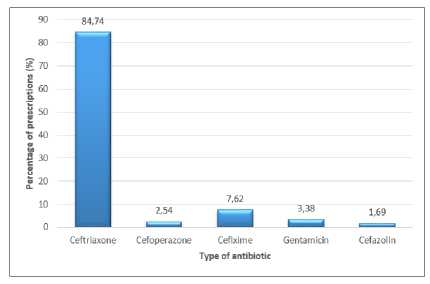
Figure 1. The pattern of Antibiotic Use for Orthopedic Surgery Based on Number of Prescriptions
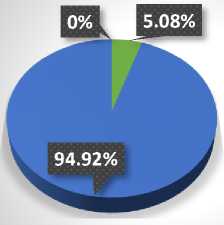
94.92%
5.08%
0%
■ Access
■ Watch
■ Reverse
Figure 2. The pattern of Orthopedic Surgical Antibiotic Use Based on Prescribing Restrictions from the WHO AWaRe Classification
DISCUSSION
Every surgical procedure has the potential for surgical site infection (SSI). If this infection occurs, it can result in morbidity and mortality in patients, which results in increased treatment costs and prolonged hospital stays. To prevent the occurrence of that post-surgical infectious complications, surgical patients are generally given antibiotic therapy. The use of antibiotics is generally divided into three types. There are empirical, definitive
and prophylactic. Empirical use is antibiotics that are used to treat infections in general before the microorganism that causes the infection is identified and the specific antibiotics to be used are known. A definitive antibiotic is an antibiotic that is specific to the microorganism that causes the infection. Prophylactic antibiotics are used to prevent possible infections, usually in surgical procedures[5]. The selection of antibiotic therapy used is based on the guidelines for
the use of antibiotics that have been prepared by each hospital based on the results of the germs map in each hospital.
The research results obtained 45 patient medical records that were used as research samples. Based on Table 1, it can be seen that the age group of patients most commonly diagnosed with orthopaedic surgery was the age group 18-24 years, with as many as 13 cases (28.89%). This result is in accordance with the results of Indonesia's health research (2018), in which the highest incidence of injury occurs at the age of 15-24. Table 1 shows that more orthopaedic surgery patients are male than female. These results are in accordance with the results of Indonesia health research (2018), which shows that the incidence of injuries and traffic accidents which often require orthopaedic surgery occurs more frequently in males than females[6].
Based on the distribution of patient history, 95.56% of patients did not have a history of the disease. There was one patient who had a history of hypertension and one person with pneumonia. Medical history is a history of physical ailments that the patient had previously suffered to find out their association with the current illness and as material for consideration in the selection of actions to be taken. Patients who have a history of pneumonia are suspected to be known while in the hospital, so these patients receive polypharmacy treatment.
Based on Table 2, successively from most to least prescribed antibiotics were ceftriaxone (84.74%) at doses of 1 and 2 grams; cefixime (7.62%) at doses of 100 and 200 mg; gentamicin (3.38%) doses of 40 and 80 mg; cefoperazone (2.54%) doses of 1 and 2 grams; and cefazoline (1.69%) at a dose of 1 gram. Antibiotic therapy for orthopaedic surgery is generally cephalosporin group, and if the patient is allergic to this group, gentamicin can be used. Cephalosporins are broadspectrum antibiotics that work by inhibiting bacterial cell wall synthesis.
Cefazoline is a first-generation cephalosporin which is active against gram-positive bacteria. Ceftriaxone, cefoperazone and cefixime are third-generation cephalosporins which are less active against gram-positive cocci than the first generation but much more active against Enterobacteriaceae, including penicillinase-producing strains. Ceftriaxone has a longer half-life than other cephalosporins, so once a day is sufficient and is usually indicated for severe infections[7].
The use of antibiotics based on prescription restrictions in hospital formularies also needs to be carried out to implement policies on the use of antibiotics[8]. Restrictions on prescribing antibiotics in hospitals are divided based on the AwaRe (Access, Watch, and Reserve) classification from WHO recommendations. Based on Figure 2, it was found that in orthopaedic surgery, there were no antibiotics belonging to the reserve category, but the highest percentage was in the watch category (94.92%), and in the access category, it was 5.08%. This relates to the number of prescriptions for ceftriaxone which is most widely used in orthopaedic surgery. Watch category antibiotics are only used for special indications or when access group antibiotics are ineffective. Watch category may only be prescribed based on the guidelines for the use of antibiotics prepared by the Antibiotic Control Committee or after going through discussions with appointed "experts". This group has higher capabilities and the potential to generate resistance, so it is prioritized as the main target of the monitoring program. An antimicrobial resistance prevention program can be influenced by doctors' level of adherence (compliance) in prescribing antibiotics in accordance with hospital antibiotic use guidelines[9].
Cephalosporins 3rd generation overused can cause resistance through a mechanism of Extended Spectrum Beta
Lactamase (ESBL) formation. Results analysis conducted by Muro et al. (2012)[10] shows that the use of broadspectrum cephalosporins, including third-generation cephalosporins, is a significant risk factor that can trigger the occurrence of infection caused by ESBL-producing bacteria. When 3rd generation cephalosporins resistance mechanisms have been formed, the choice of antibiotics that can be used to treat patients becomes fewer, and generally, these antibiotics of choice are more expensive[11].
CONCLUSION
During the period from January to August 2022, a total of 118 antibiotics were prescribed with five types from 45 orthopaedic surgery patients, of which is ceftriaxone was the most prescribed antibiotic (84.74%). The use of antibiotics based on the AWaRe classification shows there are no antibiotics belonging to the reserve category. However, the watch category obtained the highest percentage (94.92%) and as much as 5.08% of antibiotics in access category. The description pattern of antibiotic use indicates that there is still non-selective use of antibiotics in this hospital, so in the future, it is necessary to evaluate qualitatively and quantitatively to ensure rational use as well as efforts to prevent the occurrence of antibiotic resistance in hospitals.
CONFLICT OF INTEREST
There is no conflict of interest in the preparation of this article. This article was written independently by the author without the involvement of any third party or party.
ACKNOWLEDGEMENTS
The authors would like to thank the director of the relevant hospital and the Chancellor of Udayana University through the Pharmacy Study Program, Faculty of Mathematics and Natural
Sciences, Udayana University for facilitating and funding this research.
REFERENCE
-
1. Kemenkes RI. Sistem Surveilans Resistensi Antimikroba di Indonesia dalam Penerapan GLASS. Jakarta: Kementerian Kesehatan Republik Indonesia; 2020.
-
2. Waridiarto DS, Priambodo A, Lestari ES. Kualitas penggunaan antibiotik pada kasus bedah orthopedi di bangsal bedah RSUP Dr. Kariadi. Doctoral dissertation. Faculty of Medicine; 2015.
-
3. Menkes RI. Peraturan Menteri Kesehatan Republik Indonesia Nomor 28 Tahun 2021 tentang Pedoman Penggunaan Antibiotik. Jakarta: Menteri Kesehatan Republik Indonesia; 2021.
-
4. WHO. WHO releases the 2019 AWaRe Classification Antibiotics; 2019 [cited 2022 Oct 21]. Available from:
https://www.who.int/news/item/01-10-2019-who-releases-the-2019-aware-classification-antibiotics
-
5. Gyssens IC. Audit for Monitoring The Quality of Antimicrobial Prescription. New York: Kluwer Academic Publishers; 2005.
-
6. Badan Penelitian dan Pengembangan Kesehatan Kemenkes RI. Riset
Kesehatan Dasar (RISKESDAS). Jakarta: Kementerian Kesehatan
Republik Indonesia; 2018.
-
7. BPOM RI. 5.1.2.1 Sefalosporin; 2015 [cited 2022 Nov 3]. Available from: https://pionas.pom.go.id/ioni/bab-5-infeksi/51-antibakteri/512-sefalosporin-dan-antibiotik-beta-laktam-lainnya/5121
-
8. Kemenkes RI. Peraturan Menteri Kesehatan Republik Indonesia nomor 2406/Menkes/Per/XII/2011, tentang Pedoman Umum Penggunaan
Antibiotik. Jakarta: Kementerian
Kesehatan Republik Indonesia; 2011.
-
9. Fauzia D. Strategi Optimasi
Penggunaan Antibiotik. JIK. 2015; 9:55-64.
-
10. Muro S, González G, Ortiz C, González GM, Diaz LJM, Bosques F, et al. Risk Factors Associated with Extended-Spectrum Β-Lactamase Producing Enterobacteriaceae
Nosocomial Bloodstream Infections in a Tertiary Care Hospital: a Clinical and Molecular Analysis.
Chemotherapy. 2012; 58:217-224.
-
11. Monica S, Irawati S, Setiawan E. Kajian Penggunaan, Ketepatan, dan Biaya Antibiotik pada Pasien Rawat Inap Anak di Sebuah Rumah Sakit Umum di Surabaya. Jurnal Farmasi Klinik Indonesia. 2018; 7:194-208.
81
Discussion and feedback