Extranodal Non-Hodgkin’s Lymphoma at Maxillofacial Bone: A Case Report
on

DIRECTORY OF
OPEN ACCESS
JOURNALS

Extranodal Non-Hodgkin’s Lymphoma at Maxillofacial Bone: A Case Report
Thomas Arie Satya Wardhana1, Putu Anda Tusta Adiputra2*
1General Surgery Training Programme, Faculty of Medicine Udayana University, Sanglah General Hospital Denpasar, Bali, Indonesia.
2Oncology Surgery Division, Surgery Department, Faculty of Medicine Udayana University, Sanglah General Hospital, Denpasar, Indonesia.
*Corresponding author: andatusta@unud.ac.id.
ABSTRACT
Background: Extranodal lymphoma appears in about 40% of all lymphoma patients and has been reported in almost all tissue and organs. The most common site is the intestinal tract, followed by head and neck. There are many reports about extranodal lymphomas that arise in orbits, paranasal sinus and oral cavities, nasal, thyroid and salivary glands. These lymphomas usually do not destroy adjacent bone, unlike squamous cell carcinoma. Case: We would like to present an uncommon case of diffuse large B-cell extranodal lymphoma arising maxillofacial bone on buccal area that infiltrating to maxillary sinus and orbital, with bone destruction as well. The patient responded well with CEOP regimen chemotherapy and showed significant tumor regression with symptoms reduction. She just underwent the seventh series of chemotherapy now and planned to be restaging after eighth chemotherapy. Conclusion: Chemotherapy remains the treatment of choice for non-Hodgkin lymphomas. Surgery also takes place in modality choice of treatment of maxillary cancer, either a partial or total maxillectomy alone, or maxillectomy with craniofacial resection.
Keywords: extranodal lymphomas, maxillofacial bone, CEOP regimen.
DOI: https://doi.org/10.24843/JBN.2019.v03.i02.p02
INTRODUCTION
Extranodal lymphoma occurs in about 40% of all lymphoma patients and has been reported in almost all tissue and organs. It is more common with non-Hodgkin's lymphoma (NHL), with subtype diffuse large B-cell lymphoma (DLBCL), about 25% of all NHL patients.1 The most common site is the intestinal tract, followed by head and neck. The most common site found at head and neck is in the Waldeyer’s ring, nasal, sinus, orbit, and oral cavities, thyroid and salivary glands.1,2 Extranodal NHL at the head and neck region differ from SCC that usually destroys involved bone, which does not occur in NHL. DLBCL primarily arising at maxillofacial bone has been rarely reported.1
We would like to report a rare case of a woman with primarily DLBCL which located
at the maxillofacial bone on the buccal area that infiltrating to the maxillary sinus and orbital, with bone destruction.
CASE REPORT
A 60-year-old female presented with a 4-month history of solid mass at her left buccal area that enlarged rapidly. She also felt pain at her left upper jaw and left orbit. There was no history of prolonged sunlight exposure or skin tumor from her side of family. The patient’s weight remained unchanged.
Physical examination revealed an ill-defined fungating mass at her left buccal region, with hard consistency and fixed to the maxillar bone, with no ulcer. No lymph nodes were palpable. We found no significant at other physical examination. The peripheral blood count was within the normal limit
37 | JBN (Jurnal Bedah Nasional)
(hemoglobin 10.9 g/L, red blood cell count 3.81x1012/L, white blood cell count 3.05x109/L, and platelet count 230x109/L). Liver and renal functional tests, bilirubin, and electrolytes were normal. LDH serum was also within the normal limit (359 U/L).
The skull X-ray was obtained, which showed the left maxillofacial bone became more blastic and thinner. We proceeded with contrast-enhanced CT scan which revealed solid mass at the left maxillofacial bone which infiltrating to left facial-buccal area, left maxillary sinus and left orbit, with bone destruction (Figure 1 and Figure 2). There was no infiltration to the intracranial area. There was no extranodal involvement of the lung, pleura, and liver.
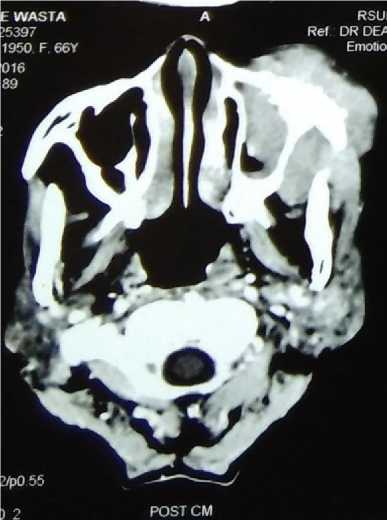
Figure 1. Head CT axial view.
The patient was undergone intraoral biopsy and assessed with non-Hodgkin’s lymphoma, predominantly large cell, and continued to be checked with lymphomas panels, which in our hospital policy only covered CD20, and showed negativity for CD20. DLCBL was the final confirmed diagnosis.
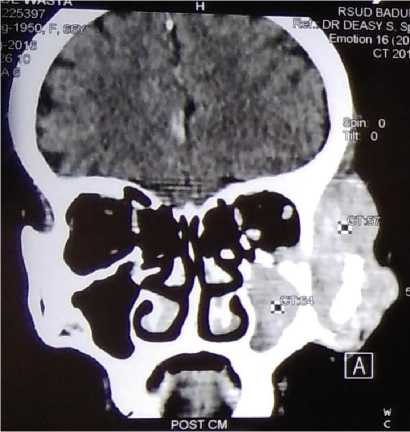
Figure 2. Head CT coronal view.
The patient was treated with CEOP chemotherapy for seven out of eight series planned and showed a good partial response, the tumor shrank significantly (Figure 3), and the pain was reduced dramatically. The patient was planned to receive eight series of CEOP chemotherapy and get restaging afterward.

Figure 3. Clinical picture of the patient after 7 series of chemotherapy.
DISCUSSION
DLBCL is the most common type of lymphoma worldwide. With the high percentage of extranodal involvement (40%), physicians must aware of this kind of tumor,
and do the workup accurately. While most of the extranodal non-Hodgkin lymphomas occur in the intestinal tract, a quarter of those occur in head and neck region.1,3 There has been reported on cases extranodal nonHodgkin lymphomas occur at retroperitoneal space, central nervous system, even presenting atypically as periprosthetic joint infection.2 This is a unique case of extranodal non-Hodgkin’s lymphoma which occur at the maxillofacial bone with the destruction of the bone.
While complete history-taking and physical examination are still the first approaches to diagnose the patient, radiologic imaging is also taking important role to give the accurate diagnosis in extranodal lymphomas, especially CT scan in maxillary or paranasal sinus involvement.4 CT and MRI usually show opacification of the sinus, bone destruction, and invasion of adjacent structures, which are presents on our patient. MRI is superior from CT because can evaluate soft-tissue better, depends on the site of the extranodal tumor.4,5 Definitive histological diagnosis is needed from biopsy or tumor resection in order to give the appropriate treatment.
The current treatment of choice for DLBLC is CHOP chemotherapy. And the combination CHOP with rituximab has become the gold standard of therapy. Rituximab is a chimeric anti-CD20 IgG1 monoclonal antibody which is a cell surface protein that occurs almost exclusively in mature B-cells. 6 However, the anthracycline component of R-CHOP propose high risk because of its toxicity in frail older patients or those with underlying cardiac dysfunction. The prognosis has improved in recent years regarding the vast development of chemotherapeutic regimens which are given appropriately with considering on the histological type, stage, and age of each
patient. Hence, a definitive histological diagnosis is at utmost importance for patients with DLBLC.6,7
R-CEOP, with doxorubicin replaced by etoposide (50 mg/m2 IV on day 1 and 100 mg/m2 PO on days 2 and 3) is an alternative regimen for older patients or patients ineligible for anthracyclines. Moccia et al. (2009) reported the efficacy of R-CEOP in R-CHOP-ineligible DLBCL patients and compared their outcomes to a historical cohort receiving R-CHOP.2 Although patients treated with R-CEOP had a lower 5-year OS rate than the R-CHOP group (49% vs. 64%, respectively; p=0.02), the 5-year time to progression rate was similar in both groups (57% for R-CEOP vs. 62% for R-CHOP; p=0.21). These results suggest that R-CEOP may be an alternative, potentially curative treatment for patients whose risk factors preclude them from receiving R-CHOP. As for our patient, CEOP was given because of consideration of older age, and underlying cardiac dysfunction. Another choice of chemotherapy regimens including CEOP + filgrastim, high-dose clarithromycin, high-dose methotrexate, etoposide, dexamethasone and pegaspargase (MEDA).6,8
CONCLUSION
While chemotherapy remains the treatment of choice for non-Hodgkin lymphomas, radiotherapy is regarded as primary treatment for early-stage extranodal lymphoma, nasal type and must be put into consideration when choosing the modality of treatment. Surgery also takes place in modality choice of treatment of maxillary cancer, which can be used as adjuvant therapy in addition to chemotherapy, or vice versa. Surgery approach for these cases (maxillary cancer) would be either a partial or total maxillectomy alone or maxillectomy with craniofacial resection.
ACKNOWLEDGEMENT 5.
None.
DISCLOSURE
Authors declare no conflict of interest of this report. 6.
REFERENCES
-
1. Cai YL, Xiong XZ, Lu J, et al. NonHodgkin’s lymphoma with uncommon clinical manifestations: A case report.
Oncol Lett. 2015;10:1686-8. 7.
-
2. Rajeev A, Ralte A, Choudhry N, et al. Diffuse B Cell Non-Hodgkin’s Lymphoma Presenting Atypically as Periprosthetic Join Infection in a Total Hip Replacement. Case Reports in Orthopedics. 2017;2017:7195016.
-
3. Bao YY, Yong WW, Han HM, et al. Diffuse large B-cell lymphoma of the 8. maxillary sinus in a patient with acquired immunodeficiency syndrome. Int J Clin Exp Med. 2016;9:12227-32.
-
4. MacDonald D, Li T, Leung SF, et al. Extranodal lymphoma arising within the maxillary alveolus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124:e233-8.
Ramanathan A, Mahmoud HA, Hui LP, et al. Oral Extranodal non Hodgkin’s lymphoma: series of forty two cases in Malaysia. Asian Pac J Cancer Prev. 2014;15:1633-7.
Rashidi A, Oak E, Carson KR, et al. Outcomes with R-CEOP for R-CHOP-ineligible patients with diffuse large B-cell lymphoma are highly dependent on cell of origin defined by Hans criteria. Leuk Lymphoma. 2016;57:1191-3.
Hertzberg M, Matthews JP, Stone JM, et al. A phase III randomized trial of high-dose CEOP + filgrastim versus standarddose CEOP in patients with non-Hodgkin lymphoma: 10-year follow-up data: Australian Leukaemia and Lymphoma Group (ALLG) NHL07 Trial. Am J Hematol. 2014;89:536-41.
Jiang, L, Li, SJ, Jiang, YM, Long, JX, Wang, RS, Su, J, Zhang, Y: The significance of combining radiotherapy with chemotherapy for early stage extranodal natural killer/T-cell lymphoma, nasal type: a systematic review and meta-analysis. Leuk Lymphoma. 2014;55:1038-48.
40
Discussion and feedback