Prevalence and Characteristic of Superficial Fungal Infection in Denpasar City, Bali, Indonesia
on
INTERNATIONAL JOURNAL OF BIOSCIENCES AND BIOTECHNOLOGY eISSN: 2655-9994 pISSN: 2303-3371
Vol. 11 No. 1 September 2023

Prevalence and Characteristic of Superficial Fungal
Infection in Denpasar City, Bali, Indonesia
I Gde Nengah Adhilaksman Sunyamurthi Wirawan1*, I Made Indra Wijaya2
1Department of Professional Medicine, Faculty of Medicine and Health Sciences, Warmadewa University, Terompong St., No. 24, Denpasar, Bali, 80239, Indonesia
-
2Department of Community Medicine - Preventive Medicine, Faculty of Medicine and Health Sciences, Warmadewa University, Terompong St., No. 24, Denpasar, Bali, 80239, Indonesia
-
*Correspondence email: moaixmoai@gmail.com
Received: 06-23-2023 Revised: 10-30-2023 Accepted: 11-31-2023
Citation: Wirawan, I.G. & Wijaya, I.M.I.. (2023). Prevalence and Characteristic of Superficial Fungal Infection in Denpasar City, Bali, Indonesia. International Journal of Biosciences and Biotechnology, 11 (1): 1-7.
https://doi.org/10.24843/IJBB.2023.v11.i01.p01.
Abstract. Superficial mycoses are the most common dermatological diseases caused chiefly by dermatophytes. Due to poor hygiene, superficial mycosis is more common in rural areas, yet the disease can also spread in urban areas. This study aims to determine the prevalence of superficial mycoses and compare the characteristics of skin lesions with the results of a microscopic examination of the fungus. According to this study, Pityriasis versicolor (22.2%), Tinea corporis (35.8%), and Tinea cruris (25.3%) were the three most prevalent superficial mycoses. The age distribution revealed that 25.4% of the samples were obtained from children, 37.3% from young adults, 25.4% from middle-aged adults, and 11.9% from old adults. Results from microscopic examination suggest that hyphae were absent in 28.4% of samples suspected of having an infection with superficial mycoses. In this study, the short hyphae of Malassezia and the septate and hyaline hyphae of dermatophytes could be distinguished.
Keywords: Characteristic Infection, Dermatophytosis, Prevalence, Tineas
Diseases caused by fungi are prevalent and ubiquitous, particularly in tropical regions. Superficial mycoses are the most prevalent dermatological diseases, caused primarily by dermatophytes and, in some cases, nondermatophyte filamentous fungus, such as Pityriasis versicolor from the genus Malassezia (Buil et al., 2020; Oke et al., 2014). Dermatophyte fungi infect keratinized tissue, such as the skin and its appendages. It is sufficient for dermatophyte spores to initiate germination and infect skin cells, particularly keratin-rich stratum layers, when there is a certain amount of moisture. The spores on hair or under the nail plate can cause infection. Thus, dermatophytosis is considered a superficial infection (Hussein and AL-Janabi, 2014). Pathogenic species in this group are anthropophilic, zoophilic, and geophilic fungi belonging to the genera Trichophyton, Microsporum, and Epidermophyton (de Hoog et al., 2017).
Central Laboratory for Genetic Resource and Molecular Biology
Faculty of Agriculture Udayana University
https://ojs.unud.ac.id/index.php/jbb/index
Tineas are diseases that occur from a dermatophyte infection. Tinea pedis refers to dermatophyte infections of the foot, Tinea cruris to infections of the genitalia; Tinea corporis to trunk infections, and Tinea capitis to scalp infections. There are at least 40 human-infecting species of dermatophytes, and several of these fungi can cause disease in many body sites (White et al., 2014).
According to (Rahman et al., 2011), superficial mycosis is more prevalent in rural regions due to a lack of hygiene, although this does not preclude the disease from spreading in cities. This research is an analytic study that aims to measure the prevalence of superficial mycoses and compare the characteristics of skin lesions with the results of a microscopic investigation of the fungus.
This study comprised patients from a clinic in Denpasar City, the capital of Bali Province, Indonesia. The data collection was conducted from November 2022 to January 2023, with 67 patients from Denpasar city. Patients suspected of having superficial mycosis underwent a skin scraping test for fungal infection. The specimens were placed aseptically on a glass slide with 10% KOH and examined under a microscope for fungal hyphae and spores. The microscope used is fluorescence microscope from the Lab of Genetic Resources, Udayana University, Denpasar, Bali, Indonesia. The microscope was connected to a computer, so that, its can be edited for making a better imaged. The microscope used was Nikon ECLIPSE 50 and Nikon SMZ 1500. Some samples were subjected to culture on Potato Dextrose Agar (PDA) media for 1-2 days and then the formed of hyphae and spores were observed and then confirmed under microscope. The PDA media was purchased from the Genetika Science Indonesia (GSI). The identified data were then tabulated and grouped into species of fungi and in age groups of the samples.
This study comprised 67 individuals diagnosed with superficial fungal infection; 53.7% were male, and 46.3% were female. The most common superficial mycoses were Tinea corporis (35.8%), Tinea cruris (25.3%), and Pityriasis versicolor (PVC) (22.2%), as shown in Table 1. Tinea pedis represented 6% of cases, while tinea capitis and tinea facialis accounted for only 1.5%. Additionally, 7.5% had double infections.
Table 1. Prevalence of mycosis superficial infection in male, female, and total patients
|
Fungal Infection |
Male n (%) |
Female n (%) |
N (%) |
|
Tinea corporis |
8 (11.9) |
16 (23.9) |
24 (35.8) |
|
Tinea capitis |
1 (1.5) |
0 (0.0) |
1 (1.5) |
|
Tinea pedis |
1 (1.5) |
3 (4.5) |
4 (6.0) |
|
Tinea cruris |
11 (16.4) |
6 (8.9) |
17 (25.3) |
|
Tinea facialis |
1(1.5) |
0 (0.0) |
1 (1.5) |
|
Pityriasis versicolor (PVC) |
11 (16.4) |
4 (6.0) |
15 (22.4) |
|
Tinea capitis + Tinea cruris |
1 (1.5) |
0 (0.0) |
1 (1.5) |
|
Tinea corporis + Tinea cruris |
1 (1.5) |
2 (3.0) |
3 (4.5) |
|
PVC + Tinea cruris |
1 (1.5) |
0 (0.0) |
1 (1.5) |
|
Total |
36 (53.7) |
31 (46.3) |
67 (100) |
Distribution of age revealed that 25.4% of samples were collected from children ages 3 to 16 years, 37.3% from young adults aged 17 to 30 years, 25.4% from middle-aged adults aged 31 to 45 years, and 11.9% from old adults aged above 45 years as shown in Table 2. Tinea corporis (14,9%) was more prevalent in middle-aged adults; Tinea capitis and Tinea facialis were only observed in children; Tinea pedis (4.5%) and Tinea cruris (10,4%) were more prevalent in young adults; and PVC (8,9%) was equally prevalent in children and young adults. Only children had a double infection of Tinea capitis and Tinea cruris; one young adult, one middle-aged adult, and one old adult had a double infection of Tinea corporis and Tinea cruris; and only children had a double infection of PVC and Tinea cruris. Meanwhile Table 3 shows microscopic examination of mycosis superficial infection. The result indicates that 28.4% of samples with a suspected infection of superficial mycoses were negative upon microscopic examination.
Table 2. Prevalence of mycosis superficial infection based on age group
|
Fungal Infection |
Age group n (%) |
N (%) | |||
|
Children -teenager (3-16) |
Young Adults (1730) |
Middle-aged Adults (3145) |
Adults (>45) | ||
|
Tinea corporis |
4 (6.0) |
8 (11.9) |
10 (14.9) |
2 (3.0) |
24 (35.8) |
|
Tinea capitis |
1 (1.5) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (1.5) |
|
Tinea pedis |
1 (1.5) |
3 (4.5) |
0 (0.0) |
0 (0.0) |
4 (6.0) |
|
Tinea cruris |
2 (3.0) |
7 (10.4) |
5 (7.5) |
3 (4.4) |
17 (25.3) |
|
Tinea facialis |
1 (1.5) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (1.5) |
|
PVC (Pityriasis versicolor) |
6 (8.9) |
6 (8.9) |
1 (1.5) |
2 (3.0) |
15 (22.4) |
|
Tinea capitis + Tinea cruris |
1 (1.5) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (1.5) |
|
Tinea corporis + Tinea cruris |
0 (0.0) |
1 (1.5) |
1 (1.5) |
1 (1.5) |
3 (4.5) |
|
PVC + Tinea cruris |
1 (1.5) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (1.5) |
|
Total |
17 (25.4) |
25 (37.3) |
17 (25.4) |
8 (11.9) |
67 (100) |
Table 3. Microscopic examination of mycosis superficial infection
|
Fungal Infection |
N (%) |
Positive |
|
Tinea corporis |
24 (35.8) |
17 (25.3) |
|
Tinea capitis |
1 (1.5) |
0 (0.0) |
|
Tinea pedis |
4 (6.0) |
2 (3.0) |
|
Tinea cruris |
17 (25.3) |
12 (17.9) |
|
Tinea facialis |
1 (1.5) |
1 (1.5) |
|
PVC (Pityriasis versicolor) |
15 (22.4) |
13 (19.4) |
|
Tinea capitis + Tinea cruris |
1 (1.5) |
0 (0.0) |
|
Tinea corporis + Tinea cruris |
3 (4.5) |
2 (3.0) |
|
PVC + Tinea cruris |
1 (1.5) |
1 (1.5) |
|
Total |
67 (100) |
48 (71.6) |
The microscopic examination revealed that dermatophytes fungi were prevalent; these fungi have septate and hyaline hyphae as shown in Figure 1. However, as it is challenging to distinguish microconidia, macroconidia, and arthroconidia in the majority of samples, the genus of the fungi cannot be determined. On PVC samples, short hyphae of Malassezia were found.
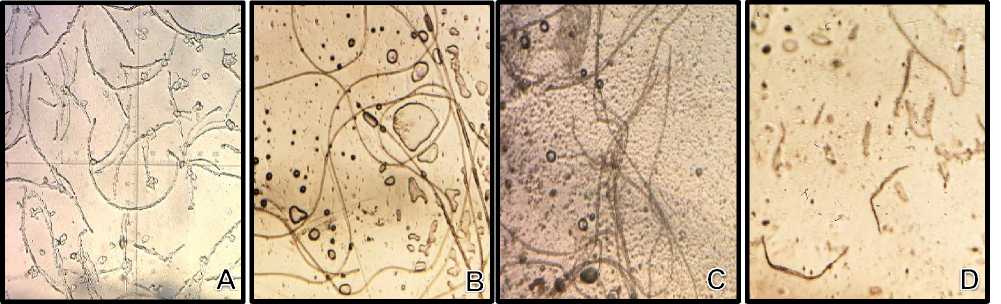
Figure 1. Fungal hyphae from microscopic examination. (A,B,C) Dermatophytes; (D) Malassezia
In this study, mycosis superficial was more prevalent in males than in females. This result is likely attributable to the protective effects of androgenic hormones in women, specifically progesterone and estradiol, which are present in more significant quantities in women than in men. These hormones can suppress skin fungus growth (Heidrich et al., 2015). Berenji et al. (2016) also observed that males had a greater prevalence of superficial mycosis. Personal hygiene, occupational activity, and exposure to contaminating agents are some factors that can influence gender predominance (Zareshahrabadi et al., 2021).
Tinea corporis was the most prevalent case of superficial mycosis in this investigation, as measured by the frequency of each occurrence. Tinea cruris and PVC represent the second and third most prevalent cases. Tinea corporis causes lesions on the trunk, the neck, the arms, and the legs. In the past seventy years, Trichophyton rubrum has been the most prevalent species causing dermatophyte diseases (Yee and Aboud, 2022). The fungus transmission is aided by a damp, warm environment, sharing towels and clothing, and wearing occlusive garments (Leung et al., 2020). Because Indonesia has a tropical climate with significant humidity, the prevalence of dermatophyte skin diseases is exceptionally high (Putri and Astari, 2017). According to Ebrahimi et al. (2019), Tinea corporis is most prevalent in tropical areas.
In this study, Tinea cruris is the second most frequent superficial mycosis. Based on age category, young adults are most susceptible to Tinea cruris. According to Yadav et al. (2013), adult males are more prone to Tinea cruris than females and children. According to research by Devy and Ervianti (2018), the incidence rate of Tinea cruris and/ or Tinea corporis is as high as 46.2% in the third and fourth decades of life. Based on profession, most instances of Tinea corporis and Tinea cruris often affect private employees (Sanggarwati et al., 2021). Without improved personal hygiene, individuals run the danger of developing dermatophytosis due to their strenuous daily activities that induce perspiration (Sodakh et al., 2016). In addition, heated climatic circumstances, heavy perspiration, and tight clothes are the triggers for Tinea corporis and Tinea cruris infections, which are present in all age groups and occupations. Additionally, genetics might render an individual more sensitive to dermatophytes (Gupta et al., 2017).
Pityriasis versicolor (PVC) or Tinea versicolor is a persistent superficial fungal disease on the trunk and upper arms characterized by round to oval lesions (White et al., 2014). Malassezia furfur and other Malassezia species mainly cause PVC infection on the stratum corneum of the skin (Kambil, 2017). This disease is connected with warm, humid conditions and is up to 60% more frequent in tropical regions than in temperate ones.
Krishan et al. (2015) reported that PVC is most prevalent in teens and young adults when sebaceous gland activity is at its peak. Malassezia requires the sebum produced by sebaceous glands for its metabolism. Typically, sebum is present on the face, scalp, chest, and back (Ahronowitz and Lesie, 2019). Sebum production in children is not yet optimal due to the small number of sebaceous glands, which will increase in number beginning with puberty (Nura et al., 2017; Remya and Arun, 2019).
In this study, mycosis superficial is most frequent in young individuals between the ages of 17 and 30. This conclusion is consistent with the findings of Khodadadi et al. (2021), who found that mycosis superficial was more frequent in individuals aged 21 to 40 years. Young adults have more outdoor working activities and are more likely to be exposed to fungal agents. Young adults are also more concerned about their health and attractiveness; therefore, they visit the hospital.
As demonstrated in Figure 1 (B), there were single-cell microconidia, which are characteristic of Trichophyton, but no macroconidia were observed. Figure 1 (D) shows the short hyphae that are characteristic of Malassezia that are responsible for PVC. Epidermophyton, Trichophyton, and Microsporum are the three closely related genera that make up the Dermatophyta and are separated into subgroups depending on the development and shape of their conidia (structures of asexual reproduction) (Hayette & Sacheli, 2015). Trichophyton spp. is one of the leading
causes of human hair, skin, and nail infections. Most Trichophyton species exhibit teleomorphic forms, which are classified within the Arthroderma genus (Ridzuan et al., 2020). The microscopic features of the fungus are septate, hyaline, conidiophores, microconidia, macroconidia, and arthroconidia. Conidiophores are challenging to differentiate from hyphae. Miroconidia is spherical or pyriform single-celled structures. Microconidia are frequently the predominant type of conidia in Trichophyton. Macroconidia is multicellular, soft, thin-walled, cylindrical, clavate, or cigar-shaped (Ridzuan et al., 2020).
Anthropophilic dermatophyte Epidermophyton spp. is widely dispersed worldwide and frequently causes onychomycosis, Tinea pedis, Tinea corporis, and Tinea cruris. Microscopically, Epidermophyton spp. exhibit septate and hyaline hyphae filamentous fungus. Hyphae are distinguished from other dermatophytes by the presence of soft, thin-walled, clavate, club-shaped macroconidia and the absence of microconidia (David, 2019).
Microsporum spp. are keratinophilic filamentous fungi belonging to the dermatophyte group. Microsporum spp. generate septate hyphae, microaleurioconidia, and macroaleurioconidia when viewed under the microscope. The conidiophores resemble hyphae. Soft, hyaline, thin-walled, unicellular, single, oval to clavate microaleuriconidia. Hyaline, roughened to echinulate, thin to thick-walled, generally fusiform, and multicellular (2-15 cells) are characteristics of macroaleuriconidia (Ridzuan et al., 2020).
Malassezia is the most common genus of fungi on healthy skin (Findley et al., 2013). Malassezia spp. are primarily found in lipid-rich anatomic regions, such as the face, scalp, and trunk (Gupta et al., 2003). M. globosa, M. restricta, M. sympodialis, and M. furfur are common Malassezia species that cause human dermatosis. M. globosa in pityriasis versicolor has been described as "spaghetti and meatballs" due to its short hyphal structures and plenty of yeasts (Clavaud et al., 2019). This short Malassezia hyphae were also discovered in our investigation.
Under a microscope, scrapings of skin treated with potassium hydroxide (KOH) will exhibit septate and branching long, thin hyphae. However, when utilizing simply KOH preparations for diagnosis, up to 15% of cases may generate false negatives (Panasiti et al., 2006). The findings of the KOH test conducted by Oktaviana et al. (2018) revealed that 85.25% of patient specimens contained hyphae structure. As a preliminary screening method, potassium hydroxide (KOH) microscopy is a quick, inexpensive, and easy procedure. This approach has a maximum sensitivity of 40%, a maximum specificity of 70%, and can give 15-30% false-negative findings (Yosella, 2015). For a more accurate diagnosis, conducting a fungal culture with SDA (Saboraud Dextrose Agar) medium is required. The gold standard for diagnosing dermatophytosis is a fungal culture, particularly if the diagnosis is uncertain and other tests produce unclear findings or if the disease is extensive, severe, or resistant to therapy (Andrews and Burns, 2008). Fungal culture can aid in the identification of fungal species (Leung et al., 2020).
The present study reveals that tinea corporis was the most frequent superficial mycosis in Denpasar, followed by tinea cruris and PVC (pityriaris versicolor). This study found that young individuals were the most susceptible to superficial mycoses. Some fungal specimens tested falsely negative after being examined under a microscope for this investigation. Nevertheless, this study was able to differentiate between dermatophytes and nondermatophytes (Malassezia).
Author Contributions
Conceptualization, IGW.; methodology, IGW.; validation, IGW.; formal analysis, IMIW.; investigation, IMIW.; resources, IMIW.; data curation, IGW.; writing—original draft preparation, IGW.; writing—review and editing, IGW. and IMIW; visualization, IMIW.; supervision, X.X IGW. and IMIW.; project administration IMIW.; funding acquisition, IGW. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Not applicable.
Data Availability
Not applicable.
Acknowledgements
The authors would like to thank the Health Research Ethics Committee of the Faculty of Medicine and Health Sciences for issuing Ethical Clearance for this research through Ethical Clearance Letter No. 22/Unwar/FKIK/EC-KEPK/III/2023.
Conflicts of Interest
The authors declare no conflict of interest
References
Ahronowitz, I., Lesie, K. (2019). Yeast Infections. Fitzpatrick’s Dermatology in General Medicine. 9th Ed. New
York: McGraw-Hill, p. 2952–63.
Andrews, M.D., Burns, M. (2008). Common tinea infections in children. Am Fam Physician, 77(10):1415–1420.
Berenji, F., Sivaki, M.M., Sadabadi, F., Aliabadi, Z.A., Ganjbakhsh, M., Salehi, M. (2016). A retrospective study of cutaneous fungal infections in patients referred to Imam Reza Hospital of Mashhad. Curr Med Mycol. 2(1): 20-23.
Buil, J.B., Meijer, E.F., Denning, D.W., Verweij, P.E., Meis, J.F. (2020). Burden of serious fungal infections in the Netherlands. Mycoses, 63(6): 625-631.
Clavaud, C., Jourdain, R., Bar-Hen, A., Tichit, M., Bouchier, C., Pouradier, F., El Rawadi, C., Guillot, J., Ménard-Szczebara, F., Breton, L., Latgé, J-P., Mouyna, I. (2013). Dandruff is associated with disequilibrium in the proportion of the major bacterial and fungal populations colonizing the scalp. PLoS One 8: e58203.
de Hoog, G.S., Dukik, K., Monod, M., et al. (2017). Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia. 182(1–2): 5-31.
Devy, D., Ervianti, E. (2018). Studi Retrospektif: Karakteristik Dermatofitosis. Berkala Ilmu Kesehatan Kulit dan Kelamin. 30(1): 66-72.
Ebrahimi, M., Zarrinfar, H., Naseri, A., et al. (2019). Epidemiology of dermatophytosis in Northeastern Iran: a subtropical region. Curr Med Mycol. 5(2): 16–21. doi.org/10.18502/cmm.5.2.1156.
Findley, K., Oh, J., Yang, J., Conlan, S., Deming, C., Meyer, J.A., Schoenfeld, D., Nomicos, E., Park, M., Kong, H.H., Segre, J.A. (2013). NIH Intramural Sequencing Center Comparative Sequencing Program. Topographic diversity of fungal and bacterial communities in human skin. Nature. 498: 367–370.
Gupta, A.K., Bluhm, R., Cooper, E.A., Summerbell, R.C., Batra, R. (2003). Seborrheic dermatitis. Dermatol Clin. 21:401–412.
Gupta, A.K., Foley, K.A., Versteeg, S.G. (2017). New Antifungal Agents and New Formulations Against Dermatophytes. Mycopathologia. 182(1-2): 127-141.
Hayette, M., Sacheli, R. (2015). Dermatophytosis, trends in epidemiology and diagnosis approach. Current fungal
Infection Reports. 9(6): 164-179.
Kambil, S.M. (2017). A Clinical and Epidemiological Study of Pityriasis Versicolor. 5(9): 155–9.
Khodadadi, H., Zomorodian, K., Nouraei, H., Zareshahrabadi, Z., Barzegar, S., Zare, M.R., Pakshir, K. (2021).
Prevalence of superficial-cutaneous fungal infections in Shiraz, Iran: A five-year retrospective study (2015– 2019). J Clin Lab Anal. 35:e23850.
Krishan, K., Badgal, A., Dogra, D., Dogra, N.K.(2015). A Single Centre Study on Epidemiological and Clinical Aspects of Pityriasis Versicolor and Prevalence of Other Dermatosis with High Sebum Production.
Leung, A.K.C., Lam, J.M., Leong, K.F., Hon, K.L. (2020). Tinea corporis: an updated review. Drugs in Context, 9.
Nura, M,S., Sani, N., Abubakar, M, AS K. 2016. A Review Of The Current Status Of Tinea Versicolor In Some Parts Of Nigeria. Int J Sci Eng Appl Sci. 2: 201–217.
Oke, O., Onayemi, O., Olasode, O., Omisore, A., Oninla, O. (2014). The prevalence and pattern of superficial fungal infections among school children in ile-ife, south-western nigeria. Dermatol Res Pract.2014: 1-7.
Panasiti, V., Borroni, R.G., Devirgiliis, V., Rossi, M., Fabbrizio, L., Masciangelo, R., Bottoni, U., Calvieri, S.
(2006). Comparison of diagnostic methods in the diagnosis of dermatomycoses and onychomycoses. Mycoses. 49(1): 26-29.
Putri, A.I., Astari, L. (2017). Profil dan evaluasi pasien dermatofitosis. Berkala Ilmu Kesehatan Kulit dan Kelamin. 29(2): 135-141.
Qadim, H. H., Golforoushan, F., Azimi, H., Goldust, M. (2013). Original papers factors leading to dermatophytosis. Annals of Parasitology. 59(2): 99–102.
Rahman, M.H., Hadiuzzaman, Jaman, M.K., Bhuiyan, Islam, N., Ansari, N.P., Mumu, S.A., Chowdhury, I.J. (2011). Prevalence of superficial fungal infections in the rural areas of Bangladesh. Iran J Dermatol. 14: 8691.
Remya, V., Arun, B. (2019). Diagnostic Efficacy of Wood’s Lamp Examination Compared with Koh Wet Mount for Diagnosis of Pityriasis Versicolor Cases. Int J Heal Sci Res. 9(4): 27–30.
Ridzuan, P.M., Nazira, C.M., Ruth, M., Rassip, C.N.A., Raihan, M.H.N., Ismail, S., Rahman, N.I.A., Suzima, E.A., Azhan, H. (2019). Mino review on dermatomycosis. J Sci Math L. 8: 6-15.
Sanggarwati, S.Y.D.R., Wahyunitisari, M.R., Astari, L., Ervianti, E. (2021). Profile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective Study. Berkala Ilmu Kesehatan Kulit Dan Kelamin. 33(1): 34–39. doi.org/10.20473/bikk.V33.1.2021.34-39.
Sondakh, C.E., Pandaleke, T.A., Mawu, F.O. (2016). Profil dermatofitosis di Poliklinik Kulit dan Kelamin RSUP Prof. Dr. RD Kandou Manado periode Januari–Desember. e-CliniC. 4(1): 1-7.
White, T.C., FIndley, K., Dawson Jr., T.L., Scheynius, A., Boekhout, T., Cuomo, C.A., Xu, J., Saunders, C.W.
(2014). Fungi on the Skin: Dermatophytes and Malassezia. Cold Spring Harb Perspect Med. 4:a019802
Yadav, A., Urhekar, A.D., Mane, V., Danu, M.S., Goel, N., Ajit, K.G. (2013). Optimization and isolation of dermatophytes from clinical samples and in vitro antifungal susceptibility testing by disc diffusion method. Journal of Microbiology and Biotechnology. 2(3):19-34.
Yee, G., Al Aboud, A. M. (2022). Tinea Corporis. In StatPearls. StatPearls Publishing.
Yossela, T. (2015). Diagnosis dan Treatment of Tinea cruris. J Majority. 4(2):122-128.
Zareshahrabadi, Z., Totonchi, A., Rezaei-Matehkolaei, A., et al. (2021). Molecular identification and antifungal susceptibility among clinical isolates of dermatophytes in Shiraz, Iran. Mycoses. 64(4): 385-393.
7
Discussion and feedback