THE RELATION BETWEEN THE NEUTROFIL LYMPHOCYTE RATIO (NLR) AND THE DEGREE OF DENGUE HEMORRHAGIC FEVER IN THE INPATIENT INSTALLATION OF ARI CANTI HOSPITAL FOR THE PERIOD OF APRIL 2022 – MAY 2023
on

ISSN: 2597-8012 JURNAL MEDIKA UDAYANA, VOL. 13 NO.01, JANUARI, 2024


Received: 2023-11-08 Revision: 2023-11-30 Accepted: 30-12-2023
THE RELATION BETWEEN THE NEUTROFIL LYMPHOCYTE RATIO (NLR) AND THE DEGREE OF DENGUE HEMORRHAGIC FEVER IN THE INPATIENT INSTALLATION OF
ARI CANTI HOSPITAL FOR THE PERIOD OF APRIL 2022 – MAY 2023
Ni Kadek Seri Mahayanti1, Ketut Suardamana2 1 General Practitioner at Ari Canti Hospital
2 Internal Medicine Specialist at Ari Canti Hospital / Department of Internal Medicine, Faculty of Medicine, Udayana University / Prof.dr.I.G.N.G Ngoerah Hospital, Denpasar e-mail:mahayantiseri@yahoo.com
ABSTRACT
Dengue Hemorrhagic Fever is caused by dengue virus infection which can cause death and cause an outbreak. Neutrophil lymphocyte ratio (NLR) is one of the cheap laboratory parameters and can predict plasma leakage in the critical period of dengue hemorrhagic fever. This study aims to determine the profile of dengue hemorrhagic fever patients and the relationship between the neutrophil lymphocyte ratio and the degree of dengue hemorrhagic fever in patients treated at Ari Canti Hospital for the period April 2022 – May 2023. This research is a retrospective analytical study with a cross-sectional approach using secondary data from archives at the Ari Canti Hospital Inpatient Installation for the period April 2022-May 2023. Data collection in the form of gender, age, neutrophil lymphocyte ratio and degree of dengue hemorrhagic fever was carried out using the convenient purposive sampling method. This study shows that the highest age group is the 26-35-year age group 35.7%, the highest gender is male 55.3% with cases of dengue hemorrhagic fever without shock 89.2% and a neutrophil lymphocyte ratio (NLR) of >2 as much as 64.2%. The result of Mann Whitney non-parametric test, showed that p value <0.0001. There is a significant relationship between NLR and the degree of dengue hemorrhagic fever in patients hospitalized at Ari Canti Hospital in April 2022, May 2023.
Keywords : dengue virus., dengue hemorrhagic fever., hospitalization., neutrophil lymphocyte ratio
INTRODUCTION
Dengue Hemorrhagic Fever (DHF) is a disease caused by the dengue virus and transmitted through the bites of Aedes aegypti and Aedes albopictus mosquitoes. The main symptoms of this disease include high fever, bleeding symptoms, and can result in outbreaks and death.1 Clinical manifestations of dengue infection can vary from asymptomatic to dengue fever with plasma leakage which can trigger a condition of perfusion disorders called dengue shock syndrome (DSS).2
The incidence of dengue fever was recorded to have increased, where in 2000 there were 505,430 cases reported, while in 2019 cases were reported to have increased by 5.2 million cases.3 In the 2021 Indonesian Health Profile, there were 103,509 cases of dengue fever with a death rate of 725 cases. The average incidence of dengue fever is 38.15 per 100,000 population in Indonesia. The average incidence of dengue fever by province in 2021 in Bali Province is 273.1 per 100,000 population with deaths due to dengue fever being 23 cases.4 Diagnostic criteria are
based on clinical symptoms and laboratory parameters such as platelets, leukocytes and hematocrit to establish a diagnosis and determine the degree of dengue fever dengue.3 Platelet count and hematocrit are often used as indicators of the development of dengue infection, whereas leukocyte count is less frequently considered in clinical 3
practice.
Neutrophil lymphocyte ratio (NLR) is a cheap laboratory parameter and has the potential to be a predictor of systemic infection and can predict plasma leakage in the critical period of dengue hemorrhagic fever. NLR is a comparison between absolute neutrophil values and absolute lymphocytes. Neutrophils are the most common type of leukocyte, accounting for 50-70% of circulating leukocytes. This type of leukocyte is twice the size of erythrocytes and is also known as polymorphonuclear leukocyte because its nucleus consists of 2 -5 lobular structures. Lymphocytes make up 20%-30% of circulating leukocytes. Lymphocytes are responsible for specific defense responses against infections through the formation of immunity and are divided into three types: B cells, T cells and natural killer
(NK) cells.5 Neutrophils and lymphocytes account for 80% of leukocytes and play a role in fighting inflammation and infection processes, so that These two types of leukocytes can be used as indicators of the immune response.6
In the febrile phase, leukocytes can show normal values or neutrophil predominance. This can be followed by the number of leukocytes decreasing rapidly and at the end of the fever phase, neutrophils will be at their lowest point. Changes in leukocytes (≤5,000 cells/mm3) and NLR (neutrophils < lymphocytes) can be used as predictors of plasma leakage in the critical phase.6,7 This research was conducted to determine the profile of dengue hemorrhagic fever patients and the relationship between the neutrophil lymphocyte ratio and the degree of dengue fever. dengue in patients treated at Ari Canti Hospital for the period April 2022 – May 2023.
MATERIALS AND METHODE
This research is classified as a retrospective analytical study with a cross-sectional approach. Data collection was carried out in July 2023. The population of this study was all patients who were treated for dengue hemorrhagic fever at Ari Canti Hospital for the period April 2022-May 2023. The sample for this study was taken through secondary data from archives of dengue fever patients who were hospitalized and met The inclusion criteria were 56 people.
The inclusion criteria for this study were patients aged ≥ 18 years who were hospitalized with dengue hemorrhagic fever with a complete blood count on the 3rd or 4th day of fever and had complete medical record data. Exclusion criteria include the presence of other infections such as bacterial infections, hematological disorders such as leukemia, thalassemia and incomplete medical record data. Data collection was carried out using the convenient purposive sampling method. Research variables included gender, age, neutrophil lymphocyte ratio and degree of dengue hemorrhagic fever.
The data were analyzed using the Shapiro-Wilk test for normality test, then a non-normal distribution was obtained so that the hypothesis test was carried out using the nonparametric Mann Whitney test. This research has received ethical approval from the Research Ethics Commission of the Faculty of Medicine, Udayana University, Number: 2023.01.2.1154.
RESULT
In this study, overall data was obtained on 56 patients who were hospitalized with dengue hemorrhagic fever and met the inclusion criteria. Data was obtained from secondary data from archives at the Ari Canti Hospital Inpatient Installation for the period April 2022 – May 2023. From the results of research on dengue hemorrhagic fever patients who met the inclusion criteria, 31 patients (55.3%) were male and 25 patients (44.6%) were male. %) female (Table 1).
In a study of 56 patients with dengue hemorrhagic fever, it was found that the most cases were in the 26-35 year age range, namely 20 cases (35.7%), followed by the 18-25 year age range, 17 cases (30.3%), 36-45 year olds. there were 10 cases (17.8%) and the age group 45-60 years was the group with the lowest number of cases, namely 16% or there were 9 cases (Table 1)
Based on the degree of dengue hemorrhagic fever, it was found that 50 people (89.2%) were patients who were hospitalized with dengue fever without shock, followed by 6 patients (10.7%) who were hospitalized because of dengue hemorrhagic fever accompanied by shock (Table 1).
The profile of dengue hemorrhagic fever patients based on the highest neutrophil lymphocyte ratio value was more than 2, namely 36 cases (64.2%). The distribution of neutrophil lymphocyte ratio values for dengue hemorrhagic fever sufferers at the Ari Canti Hospital installation in April 2022-May 2023 can be seen from (Table 1).
Table 1. Distribution of Dengue Hemorrhagic Fever Patient Profiles in the Ari Canti Hospital Inpatient Installation for the Period April 2022-May 2023
|
Profile |
N = 86 |
Percentage (%) |
|
Sex | ||
|
Female |
25 |
44.6 |
|
Male |
31 |
55.3 |
|
Age (Year) | ||
|
18-25 |
17 |
30.3 |
|
26-35 |
20 |
35.7 |
|
36-45 |
10 |
17.8 |
|
45-60 |
9 |
16 |
|
Degree of DHF | ||
|
DHF with shock |
50 |
89.2 |
|
DHF without shock Neutrophil Lymphocyte Ratio |
6 |
10.7 |
|
<0.4 |
0 |
0 |
|
0.4-0.8 |
1 |
2.3 |
|
0.8-1.2 |
3 |
5.3 |
|
1.2-1.6 |
3 |
5.3 |
|
1.6-2.0 |
13 |
23.2 |
|
>2.0 |
36 |
64.2 |
The data were analyzed using the Shapiro-Wilk test for normality test, then the data distribution was not normal, so the hypothesis test was continued with the nonparametric Mann Whitney test. In the group of dengue fever patients without shock, the mean was 3.06 with a median
Table 2. The Relationship between NLR and the Degree of Dengue Hemorrhagic Fever Infection
value of 3.00, while in the group of dengue fever patients with shock the mean was 1.3 with a median value of 1.20. In this study, a statistically significant relationship was found between the NLR ratio and the degree of dengue hemorrhagic fever <0.0001 (Table 2).
Degree of DHF
NLR
p value
|
Mean |
SD |
Min |
Max |
Med | ||
|
DHF without shock |
3,06 |
0,96 |
1,50 |
5,00 |
3,00 |
<0,0001 |
|
DHF with |
1,300 |
0,52 |
0,60 |
2,00 |
1,20 | |
shock
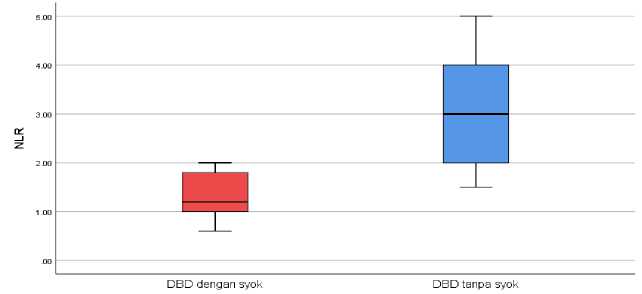
The boxplot diagram shows the distribution of patient samples, where dengue hemorrhagic fever patients with shock have a maximum value of 2.00 and a minimum
value of 0.60, while in the group of dengue hemorrhagic fever patients without shock the maximum value is 5.00 and the minimum value is 2.00 which can be seen in (Figure 1).
Status syok
Figure 1. Boxplot Comparison of NLR Values for Dengue Hemorrhagic Fever Patients with Shock and Dengue Hemorrhagic Fever Without Shock
DISCUSSION
The immune response in dengue infection involves various innate and adaptive components where the cells most involved are leukocytes, where in the early phase of dengue infection there can be a decrease in the number of leukocytes. Leukopenia is caused by suppression of myeloid progenitor cells in the bone marrow and apoptosis of immune cells. Leukopenia can be a predictor that the fever will go down and the patient will enter a critical phase. In the critical phase, the number of leukocytes will decrease (<5000 cells/mm3). This causes changes in the neutrophillymphocyte ratio due to decreased neutrophils so that the number of neutrophils is less than lymphocytes. The neutrophil lymphocyte ratio is known as a marker of infection and severe inflammation. Both neutrophils and lymphocytes play an important role in dengue virus infection. This condition is a predictor of the critical phase due to plasma leakage. These changes occur before thrombocytopenia or an increase in hematocrit.8
In dengue infection, precisely from day 3 to day 8 of fever, there will be a decrease in neutrophils which is triggered by neutrophil apoptosis due to dengue infection as well as suppression of bone marrow function either by the dengue virus or due to pro-inflammatory cytokines. Neutrophil apoptosis has a positive correlation with the severity of disease related to neutrophils having a protective function during viral infections.9 The degree of dengue fever has a significant relationship with excessive inflammation that occurs due to an excessive immune response.10 On the other hand, in dengue infection relative lymphocytosis occurs which shows the role Lymphocytes as the body's defense mechanism against dengue virus infection. The decreased neutrophil-lymphocyte ratio is caused by an increase in the number of lymphocytes and a decrease in the number of neutrophils in dengue hemorrhagic fever patients.8,9
In this study, a significant relationship was found between NLR and the degree of dengue hemorrhagic fever in patients hospitalized at Ari Canti Hospital in April 2022May 2023. This research is in accordance with research conducted at Muhamadiyah Ahmad Dahlan Hospital, Kediri in January 2019, it was found that there was a significant relationship between NLR and degree dengue hemorrhagic fever and the contingency coefficient test shows a value of -0.733, which means there is an inverse relationship where the lower the NLR, the more severe the degree of dengue hemorrhagic fever.11
The same research at RSUP Dr Kariadi and RSDN Semarang stated that there was a significant relationship between NLR in the dengue fever group and dengue hemorrhagic fever. In this study, it was found that the NLR in the dengue hemorrhagic fever patient group (mean NLR = 0.55) was lower than the dengue fever group (mean NLR = 1.23).12
Research by Jain et al., 2022 and Sadgir et al., 2022 also stated that there was a significant relationship between NLR and the degree of dengue hemorrhagic fever. In Sadgir et al., 2022 there is a relationship between NLR and platelets where NLR < 2 is highly correlated with
thrombocytopenia which indicates the severity of the disease and conversely NLR > 2 is correlated with
improvement in the degree of disease.13,14
However, research by Kristine et al., 2022, which involved children aged 0-18 years as research samples, stated that there was no significant relationship between NLR and the severity of dengue infection (p = 0.88). This is different from our research and several studies above which used samples of patients over 18 years old.15
CONCLUSION AND SUGGESTION
Based on the results of this study, it can be concluded that there is a significant relationship between NLR and the degree of dengue hemorrhagic fever in patients hospitalized at Ari Canti Hospital in April 2022 May 2023. The condition of dengue hemorrhagic fever patients becomes more severe when the NLR ratio decreases.
ACKNOWLEDGMENTS
Researchers would like to thank Dr. Ketut Suardamana, Sp.PD, K-AI as Research Supervisor and dr. I Putu Oka Dharmawan, MARS as Director of Ari Canti Hospital.
REFERENCES
-
1. Xiaorong Yang, PhD and others, Global burden for dengue and the evolving pattern in the past 30 years, Journal of Travel Medicine.2021;28(8):1-11
-
2. Avina FA, Aryati, Suhintam. Prevalence of Expanded Dengue Syndrome in Patients with Dengue Virus Infection at the Dr. Soetomo Hospital Surabaya in 2017 – 2018. Indonesia Journal of Clinical Pathology and Medical Laboratory. 2020;26(3):307-11.
-
3. WHO. Dengue and Severe Dengue Fact Sheet; WHO: Geneva, Switzerland, 2020
-
4. Nugraha KWD, Setiaji, Sibuea F, Hardhana B, Widiantini W, et al. Profil Kesehatan Indonesia 2021. Kementrian Kesehatan Republik Indonesia. 2022;214-16
-
5. Glenn, A., & Armstrong, C. E. (2019). Physiology of red and white blood cells. Anaesthesia & Intensive Care Medicine.2019;170-4
-
6. Ramadevi D, Kumar DS, Priya H. Evaluation and comparison of Neutrophil-To-Lymphocyte Ratio
(NLR) as a diagnostic marker for dengue infection. European Journal of Molecular &Clinical Medicine. 2023;10(4):752-8
-
7. Modampuri Akhil Koundinya, Dhanunjaya Dasari, S Ashok Kumar, BSV Manjula, Devi Vinaya. Neutrophil To Lymphocyte Ratio as Prognostic and Predictor Factor for Severity of Dengue Fever A Retrospective Observational Study In A Tertiary Care Centre. IAIM. 2021; 8(12): 46-52
-
8. Sugianto NA. Pathophysiology of dengue haemorrhagic fever. World Journal of Pharmaceutical Research. 2021;10(14): 218-23.
-
9. Chaloemwong J., Tantiworawit, A.,
Rattanathammethee, et al. Useful clinical features and hematological parameters for the diagnosis of dengue infection in patients with acute febrile illness; A Retrospective Study. BMC Hematology. 2018; 18 (20): 1-10
-
10. Kuczera D, Assolini JP, Tomiotto-Pellissier F, Pavanelli WR, Silveira GF.. Highlights for Dengue Immunopathogenesis: Antibody-Dependent
Enhancement, Cytokine Storm, and Beyond. J Interferon Cytokine Res. 2018. 38(2):69–80
-
11. Yuditya DC, Sudirgo Imam. The Relation Between Neutrophil Lymphocyte Count Ratio (NLCR) and Dengue Infection Grade Of Severity in Adult Patients
in RS Muhammadiyah Ahmad Dahlan Kediri in January 2019. STRADA Jurnal Ilmiah Kesehatan. 2020. 9(1): 20-5
-
12. Yuntoharjo PJI, Arkhaesi N, Hardian. Perbandingan antara Nilai Rasio Neutrofil Limfosit (NLCR) pada Anak dengan Demam Dengue dan Demam Berdarah Dengue. Jurnal Kedokteran Diponegoro.
2018. 7(2): 801-12
-
13. Jain S, Thakran BK, Chahar YK. A Cross-Sectional Study of Dengue Virus to Observe NeutrophilLymphocyte Ratio as a Predictor of Severity. International Journal of Pharmaceutical and Clinical Research. 2022; 14(12); 121-5
-
14. Sadgir A, Durge K, Masavkar S. Neutrophillymphocyte ratio as a prognostic indicator in dengue fever patients at tertiary care hospital in northwest-maharashtra. Int. J. Adv. Res. 2022. 11(01), 1198-1202
-
15. Kristine MP, Anabella SO. Absolute Neutrophil
Counts and Neutrophil to Lymphocyte Ratio as Early Predictive markers of Dengue Severity among
Children admitted in Governor Celestino Gallares Memorial Hospital: A 5- Year Retrospective Study. Acta Scientific Paediatrics 5.7, 2022: 37-45.

http://ojs.unud.ac.id/index.php/eum
doi:10.24843.MU.2024.V13.i01.P02
P a g e 11
Discussion and feedback