PARAGARD AND MIRENA AS MODERN INTRAUTERINE DEVICES
on
PARAGARD AND MIRENA AS MODERN INTRAUTERINE DEVICES
Theiva Amirta Sukantan1, I N Toya2, I G M Adioka2
Student of Medical Faculty Udayana University1, Department of Pharmaceutical Medicine, Medical School, Udayana University/ 2
Sanglah Hospital Denpasar2
ABSTRACT
There are two kinds of modern IUDs: Copper-bearing and progestin-releasing. IUD stands for IntraUterine Device, a T-shaped piece of plastic that is placed inside the uterus. The most common copper-bearing IUD is the Paragard[R] Copper T 380A. The only progestinreleasing IUD now available is Mirena[R]. The copper IUD, ParaGard, works for as long as 12 years. Copper based intrauterine devices are toxic to sperms and are also known as non-hormonal intrauterine devices. The hormonal IUD, Mirena, must be replaced after 5 years. This device functions by releasing levonorgestrel, a progestin that helps in contraception. This type of IUDs prevents the fertilization of the egg by causing sperms to become ineffective and also makes the mucus in the cervix sticky and almost impermeable. Both types make it more difficult for sperm to fertilize the egg.
Keywords: Modern contraceptive devices, Copper-bearing IUD, Hormonal IU , Fertilization
INTRODUCTION
Contraception, for both male and female can be classified into two types: terminal methods and spacing methods. Terminal methods are rather classic and include vasectomy for male and tube ligation for female. These methods aim at complete sterilization and are basically non- reversible. As for spacing methods, these are rather modern methods and are continuously being upgraded as an effect of technological advances and the main ones are pills, condom or IUD. There are basically two types of modern IUDs: copper-bearing devices and hormone releasing devices.1,5
Intrauterine devices or IUDs are devices that are used to prevent a woman from getting pregnant. IUDs are basically used as a measure for birth control. Unlike short-term options for birth control, an intrauterine device can prove to be effective for a long period of time. An IUD is a small, T-shaped plastic device that either contains hormones or is wrapped in copper. The IUD is inserted into the uterus of a woman and a plastic string from the end of the IUD hangs down
from the cervix and into the vagina. It is this plastic string that helps a woman determine if the IUD is in place. The string is also used by the doctor to remove the IUD from the uterus.3,5
It is a long-lasting and reversible method of contraception but it is not a barrier method. This means that an IUD cannot stop a person from getting sexually transmitted infections (STIs). There are different types and sizes of IUD to suit different women. IUDs need to be fitted by a trained doctor or nurse at any GP surgery, local family planning clinic or sexual health clinic.1
DESCRIPTION
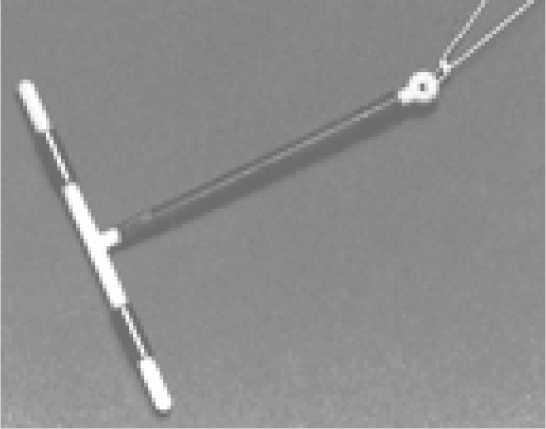
There are two kinds of modern IUDs: Copper-bearing (Paragard) and progestinreleasing (Mirena). The Mirena has a small amount of synthetic progesterone hormone that goes into the wall of the uterus. Women with this IUD usually have lighter, less painful menstrual periods. Some women with Mirena have light, irregular bleeding or spotting throughout the cycle. Others have no menstrual periods at all. A few women have mood changes, less enjoyment of sex, or headaches due to the hormones in the Mirena, but this is not common. ParaGard, has a tiny piece of wire wrapped around the plastic body. Some women choose this IUD because they want a method without artificial hormones. Most women with the ParaGard have heavier, more painful menstrual periods than before it was inserted. Some also have irregular bleeding.1,3,4,6
Fig 1 -ParaGard and Mirena.
3
Fig 1.1 The ParaGard IUD contains copper. It is effective for 12 years.3

Fig 1.2 The Mirena IUD releases a small amount of progestin, a hormone. It is effective for five years.1
TECHNIQUE OF USAGE
A physician or advanced practice clinician inserts an IUD. Some women can barely feel the insertion, which takes 5 to 15 minutes. Others find it excruciatingly painful. For most it is somewhere in between. Usually, any pain lasts only a few minutes. There may need to be a preinsertion visit for discussion and pre-testing.2
Very rarely, during insertion, the IUD can poke a hole in the uterus (perforation). Most of the time, even if this happens, the IUD is removed, and the uterus heals with no problems. In this case, the IUD could go into the abdominal cavity or become embedded in the wall of the uterus and has to be removed surgically.1,3
IUD’s can usually be removed in a few seconds. With a speculum in the woman’s vagina, the advanced practice clinician or physician simply pulls gently on her IUD string. It usually slips out easily, and sometimes the woman doesn’t even feel this. It is the patient’s right to have the IUD removed anytime she wants, for example if she wants to get pregnant or if the effects
such as bleeding or cramping are uncomfortable. A woman can use the Mirena up to five years. The ParaGard can stay in for up to ten or twelve years.1
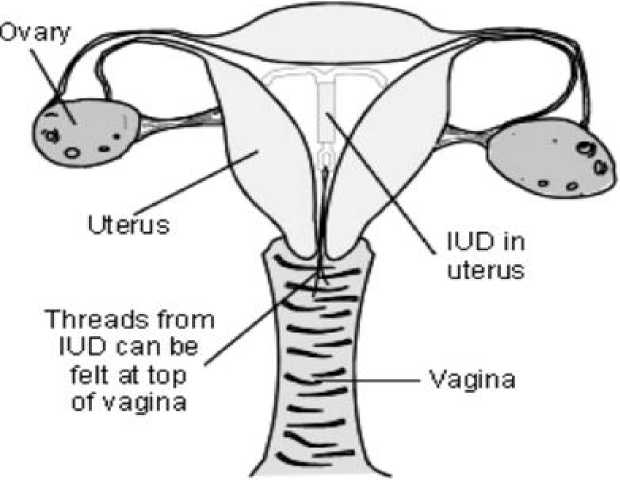
Fig 2-Simple diagram of inserted IUD and threads (used for removal) inside uterus and vagina
MECHANISM OF ACTION
Copper based devices are the most preferred intrauterine devices. The device comprises a copper wire that is wound around the stem of the T-shaped IUD. Once placed in the uterus of a woman, a copper-based device can perform its basic function for a period of at least ten years. Copper based intrauterine devices are toxic to sperms and are also known as non-hormonal intrauterine devices. Copper makes the fallopian tubes and the uterus produce a fluid that’s capable of killing sperms. The fluid contains enzymes, copperions, prostaglandins and white blood cells. The ‘Paragard T 380’ is an example of a reliable and widely used copper-based device. This explains why copper devices are so effective and popular. The T-shaped device measures 1.42 inches in the vertical direction and 1.26 inches in the horizontal direction. Sometimes, copper based devices can also come with a silver core. A silver core around a pure copper wire helps prevent the breaking of the pure copper wire, which is one of the risks associated with copper base devices. ‘Nova T 380’ is an example of a copper-based device with
a silver core. The reason why the names of all the devices comprise a number is because the number signifies the surface area of the copper in square millimeters.1,2,3,4
Hormonal intrauterine devices, also known as ‘IntraUterine Systems’, are IUDs that have an edge over copper based IUDs. These devices, unlike copper based and inert IUDs do not increase bleeding. Instead, they are effective in reducing menstrual bleeding and can sometimes even prevent the occurrence of the menstrual cycle. Hormonal devices function by releasing levonorgestrel, a progestin that helps in contraception. The IUDs prevent the fertilization of the egg by causing sperms to become ineffective and also make the mucus in the cervix sticky and almost impermeable. This makes it extremely difficult, impossible in fact, for sperms to get through to the uterus. Hormonal IUDs also prevent the lining of the uterus from thickening which makes it an improper environment for a fertilized egg. ‘Mirena’ by Bayer is an example of a widely used hormonal IUD. A hormonal IUD can prove to be effective for a period of around five years.1,2,3,4
BENEFITS OF MODERN IUDS
The ParaGard and the Mirena IUDs are two of the least expensive, longest lasting forms of birth control available to women today. There are many other benefits. IUDs may improve sex life. There is nothing to put in place before intercourse to prevent pregnancy. Some women say that they feel free to be more spontaneous because they do not have to worry about becoming pregnant. The ParaGard IUD does not change a woman's hormone levels. The Mirena IUD may reduce period cramps and make period lighter. On average, menstrual flow is reduced by 90 percent. For some women, periods stop altogether. IUDs can be used during breastfeeding. The ability to become pregnant returns quickly once the IUD is removed. Some women may worry that they are pregnant if they do not have a regular period. But the IUD is very effective. Overall, most women who get an IUD are satisfied with their choice. Ninety-nine percent of IUD users are pleased with them. 1,2,3,6
EFFECTIVENESS
Effectiveness is an important and common concern when choosing a birth control method. IUDs are one of the most effective forms of birth control available. Less than 1 out of 100 women will get pregnant each year if they use the ParaGard or the Mirena IUD.1,3
The ParaGard and Mirena IUDS can be used as emergency birth control, to prevent pregnancy after unprotected intercourse. It can reduce the risk of pregnancy by 99.9 percent if inserted within 120 hours (five days) after unprotected intercourse.1,3
COMPLICATIONS AND DISADVANTAGES
There is a very small chance of getting an infection during the first 20 days after an IUD is put in. The patient must be advised to have a check for any possible existing infection before an IUD is fitted. The IUD can be pushed out by the uterus (expulsion) or it can move (displacement).This is not common. This is more likely to happen soon after it has been put in and the patient may not know it has happened. This is why the doctor or nurse must teach the patient how to check their IUD threads every month. It is not common, but there is a risk that an IUD might go through (perforate) the uterus or cervix when it is put in. This may cause pain but often there are no symptoms. If it happens, the IUD may have to be removed by surgery. The risk of perforation is low when an IUD is fitted by an experienced doctor or nurse.4,5
The user may have cramps and a backache for the first few hours after an IUD is inserted into her uterus. Some women have bleeding and pain for a couple of weeks after the IUD is inserted. An older kind of IUD (which is no longer available) had serious side effects, including pelvic infections and infertility (problems getting pregnant after removal).4,5
The IUD does not protect users from any sexually transmitted infections (STIs). The more people the user has sex with, the greater the chance of getting an STI. The IUD alone is best for women who have only one long-term sex partner. In addition, the patient shouldn't use the IUD if she is pregnant, if she has abnormal bleeding or if she has cancer of the cervix or uterus. Most importantly, one should not use the copper IUD if she is allergic to copper.So basically, there are three main things to watch out for when using an IUD. The IUD can sometimes slip out of the uterus. Sometimes it comes all the way out. Sometimes it only comes out a little. This is more likely to happen to women who are younger and who have never had a baby. If the IUD slips out of place, pregnancy can happen. If it comes out only part of the way, it has to be removed. In rare situations, a woman could develop an infection when using the IUD. This happens if bacteria get into the uterus when the IUD is inserted. Most infections develop within three weeks of having the IUD inserted. If the infection is not treated, it can affect a woman's ability to become pregnant in the future. In very rare situations, when the IUD is
inserted, it can push through the wall of the uterus. This might sound painful, but it usually isn't. Usually, when this happens, the health care provider will notice it and it can be fixed right away. But if not, the IUD can move around and harm other parts of the body. When this happens, surgery may be needed to remove the IUD. 3,4,5,6
CONTRAINDICATION
Most women can use either the ParaGard or the Mirena IUD safely. But all medications have some risks, so safety is a common concern when choosing a birth control method. Certain conditions increase the risk of side effects. One should not use an IUD if she has had a pelvic infection following either childbirth or an abortion in the past three months, has or may have a sexually transmitted infection or other pelvic infection, thinks she might be pregnant, has cervical cancer that hasn't been treated, has cancer of the uterus, has unexplained bleeding in her vagina, has pelvic tuberculosis or has a uterine perforation during IUD insertion.
Specifically, one should not use the ParaGard IUD if she has, or may have, an allergy to copper or have Wilson's Disease — an inherited disease that blocks the body’s ability to get rid of copper. Where else, one should not use the Mirena IUD if she has severe liver disease or has, or may have, breast cancer. 1,5,6
SUMMARY
The copper-coated IUD primarily prevents pregnancy by not allowing the sperm to fertilize the egg. It may also make it harder for a fertilized egg to implant in the uterus. When an IUD is coated with progesterone, it works in a similar way, but may also thicken the cervical mucus, which prevents sperm from entering the uterus and possibly prevent ovulation (the release of an egg during the monthly cycle). Neither the plastic in the uterus nor the string in the vagina can be seen or felt. A woman can have the IUD removed whenever she wants, although she can keep it in for up to twelve years. The way it works is not completely known but it is 99.2 to 99.9% effective. In fact is it slightly more effective than sterilization. The IUD makes it harder for sperm and eggs to move, making fertilization less likely and also makes it hard for a fertilized egg to lodge in the uterus. While the IUD is very effective at preventing pregnancy, it offers no protection against sexually transmitted diseases.
The Mirena hormonal IUD functions by releasing levonorgestrel, a progestin that helps in contraception. The IUD prevents the fertilization of the egg by causing sperms to become ineffective and also make the mucus in the cervix sticky and almost impermeable. This makes it extremely difficult, impossible in fact, for sperms to get through to the uterus. The high incidence of unplanned pregnancies worldwide; especially in countries where existing contraceptives are readily available shows the inefficiency of current contraceptive methods. This has made women worldwide to prefer different types of contraceptives based on various reasons; mainly the fear of inefficiency of a particular contraceptive method. Women generally prefer contraceptives that are highly effective and do not produce adverse health effects, whether be modern and technologically advanced or not. The IUD is generally not recommended for women who have multiple sexual partners as it has no protection against STDs.
REFERENCES
-
1. Erica Weir. Preventing pregnancy: a fresh look at the IUD. CMAJ. SEPT. 16, 2003; 169
-179.
-
2. William A. Fisher, Amanda Black. Contraception in Canada: a review of method choices,
characteristics, adherence and approaches to counseling. CMAJ. 2007; 176(7): 953961.
-
3. David Grimes, Raquel Arias, Lee Shulman, Anne Moore. Intrauterine Copper
Contraceptive: Update and Opportunities. The Journal of Family Practice. 2006: S1-S8.
-
4. Karen R. Katz, Laura M. Johnson, Barbara Janowitz, José Miguel Carranza. Reasons for
the Low Level of IUD Use in El Salvador. European Heart Journal. International Family Planning Perspectives, 2002; 28(1): 26–31.
-
5. Kalyan B. Saha, D.C. Jain, Uma C. Saha. Unfolding Contraceptive Technology: Where
Indian Population Stands Today. Kamla-Raj 2006 J. Hum. Ecol. 2008; 20(2): 125-128.
-
6. David Hubacher. The Checkered History and Bright Future of Intrauterine Contraception
in the United States. Perspectives on Sexual and Reproductive Health. Volume 34. 2002.
8
Discussion and feedback