WARENESS ON DEPRESSION AMONG FIRST YEAR MEDICAL STUDENTS IN UDAYANA UNIVERSITY
on
ISSN: 2303-2197
E-Jurnal Udayana Medica,vol 1 no 2 Mei 2017
AWARENESS ON DEPRESSION AMONG FIRST YEAR MEDICAL STUDENTS IN UDAYANA UNIVERSITY
Vickram Subramaniam1, A A Sri Wahyuni2
ABSTRACT
1Medical Education
Program, 2Departement of
Psichiatry at Sanglah
Hospital
Faculty of Medicine
Udayana University
The field of medical knowledge is immense and has different stages of training which a medical student must undergo in which studies show a high prevalence of psychological morbidity during these stages. Depression is one of the most common psychological morbidity in this demographic, with prevalence of depression up to 70% in several studies. Therefore, it is important to investigate the prevalence and risk factors of depression, especially in medical students. A descriptive cross sectional study was done on the first year medical student of the Faculty of Medicine of Udayana University from November 2015 to January 2016. The samples was selected using simple random sampling. Interview using questionnaire was done on students chosen as samples, and depression status was assessed using Beck,s Depression Inventory (BDI). Of 100 samples, 68% was categorized as normal, 26% as mild mood disturbances, 3% as borderline clinical depression, 2% as moderate depression, and 1% as severe depression. Depression was more common in younger students aged 16-17 years old, female, students who lives alone, those with introverted personality, students who prefer reading and being alone, and those reported decreased body weight and sleeping difficulty.
Keywords: awareness, depression, medical student
INTRODUCTION
The World Mental Health Survey conducted in 17 countries found that the episode of those having depression in 2015 was in an average of 1 out of 20 people. In the broadest sense depression also known as major depressive disorder, is a medical illness that negatively affects how people feel, think and act. Depression is categorized as a mood disorder which causes changes in a person’s activity as well as life perception and could even cause suicides. Moreover, it is one of the leading causes of disability and is said to be a major contributor to the global burden of disease and affects people around the world.1
A typically diagnosed person with major depressive disorder experiences at least four symptoms from a list that includes changes in appetite and weight, changes in sleep and activity, lack of energy, feelings of guilt, problems thinking and making decisions, and recurring thoughts of death or suicide. Subsequently, this depressive disorder occurs without any prior history of a manic, mixed, or hypo manic episode and usually last at least 2 weeks in which these psychological problems are clearly evident.
In turn, psychological problems among students can vary from 2% to 50% and depression is said to be one of the common health concern among
the student population where at any given time, 25% of students have been reported with the symptoms of depression.2 In addition to that, Marie Dahlin (2005) showed in her study that medical students are more distressed than the general population.3
The field of medical knowledge is immense and has different stages of training which a medical student must undergo in which studies show a high prevalence of psychological morbidity during these stages.2 Additionally, a study done among the medical students of a university in Karachi, Pakistan has came out with the result where 70 % of the students are suffering from depression based on a questionnaire distributed among 142 students.4
Therefore an in depth look into depression issues with first year medical students will be explored in this research paper to further understand this issue and understand the context of why it is happening
METHODS
A descriptive cross sectional study was done on the first year medical student of the Faculty of Medicine of Udayana University from November 2015 to January 2016. The samples was selected using simple random sampling. Interview using questionnaire regarding gender, marital status,
1
accomodation, and age was done on students chosen as samples, and depression status was assessed using Beck,s Depression Inventory (BDI). Collected data was analyzed and relevant statistics was calculated using SPSS version 17.
RESULTS
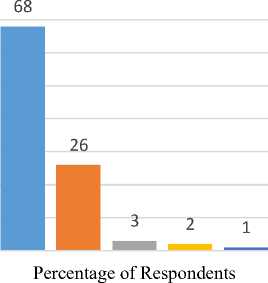
Of 100 samples, 73% of students aged between 16-18 years old, and 27% aged between 1921 years old. Based on gender, 42% was male and 58% was female. 61% of samples stayed with family, 32% with friends, and 7% stayed alone. Based on personality, 34% was introverted and 66% was extroverted. Regarding hobbies, 45% prefer hang out with friends, 29% play sports, 10% reads, and 16% prefer being alone. Based on change in body weight, 8% experience increased body weight, 22% experience decreased body weight, and 70% reported no change. 50% of samples reported sleeping early, 34% reported sleeping late, and 16% reported being unable to sleep. Based on BDI scores, 68% of samples scored 1-10, 26% scored 11-16, 3% scored 17-20, 2% scored 21-30, and 1% scored 31-40 (Table 1).
From the Figure 1 below, 68 respondents representing 68% of the total respondents have obtained a score within the range of 1-10 according to the BDI questionnaire. Thus it can be implied that these group of respondents are in the normal range as these ups and downs are considered normal. A total of 26 respondents representing 26% from the total respondents obtained a BDI score within the range of 11-16. The respondents that fall in this range of score can be said to be having mild mood disturbances, according to BDI. Apart from that, 3 (3%) respondents scored within the range of 17-20. These people suffer from borderline clinical depression. The BDI score range of 21-30 was occupied by 2 respondents with 2% from the total respondents. Those in this category are most likely to be suffering from moderate depression. And last but not least, only 1 respondent (1%) presented with a score that falls in the category of severe depression. This total of respondents represents both the male and female genders. The individual distribution of gender and BDI scores will be further discussed in this paper.
Table 1. Sample Characteristics
|
Characteristics |
Frequency |
Percentage |
|
Age (Range) | ||
|
16-18 |
73 |
73 |
|
19-21 |
27 |
27 |
|
Gender | ||
|
Male |
42 |
42 |
|
Female |
58 |
58 |
|
Living Place | ||
|
Family |
61 |
61 |
|
Alone |
32 |
32 |
|
Friends |
7 |
7 |
|
Personality | ||
|
Intovert |
34 |
34 |
|
Extrovert |
66 |
66 |
|
Hobbies | ||
|
Hang out with |
45 |
45 |
|
friends | ||
|
Play sports |
29 |
29 |
|
Read |
10 |
10 |
|
Being alone |
16 |
16 |
|
Change in Body | ||
|
Weight | ||
|
Increase |
8 |
8 |
|
Decrease |
22 |
22 |
|
No change |
70 |
70 |
|
Sleeping pattern | ||
|
Early |
50 |
50 |
|
Late |
34 |
34 |
|
Unable to |
16 |
16 |
|
sleep | ||
|
BDI Scores | ||
|
1-10 |
68 |
68 |
|
11-16 |
26 |
26 |
|
17-20 |
3 |
3 |
|
21-30 |
2 |
2 |
|
31-40 |
1 |
1 |
Figure 1. BDI Score Distribution
80
70
60
50
40
30
20
10
0
■ Scores 1-10 ■Scores 11-16 ■ Scores 17-20
■ Scores 21-30 ■ Scores 31-40
Based on age, borderline clinical depression (BDI score of 17-20) was reported by 3(7%) of students aged 17 years old. Moderate depression (BDI score of 21-30) was reported by 1(7,2%) student aged 16 years old, and 1 (2,4%) student aged 17 years old. Severe depression (BDI score of 31-40) was reported by one student aged 16 years old (Table 2).
Based on gender, borderline clinical depression was reported by 3(7,1%) male students and 1(1,7%) female student. Moderate depression and severe depression was reported by 2(3,4%) and 1(1,7%) of female students, respectively (Table 2).
Of 32 students living alone, borderline clinical depression and moderate depression was reported by 2(6,3%) students respectively, and one student reported severe depression. Of 7 students staying with friends, 1(14,3%) student reported borderline clinical depression (Table 2).
2
Based on personality, borderline clinical depression was reported by 1(6,3%) student, Table 2. BDI Scores Distribution Based On Characteristics
|
Characteristics |
1-10 |
11-16 |
BDI Score 17-20 |
21-30 |
31-40 |
Total |
|
Age | ||||||
|
16 |
8(57,1%) |
4(28,5%) |
- |
1(7,2%) |
1(7,2%) |
14 |
|
17 |
28(65,1%) |
12(28%) |
3(7%) |
1(2,4%) |
- |
43 |
|
18 |
10(66,7%) |
5(33,3%) |
- |
- |
- |
15 |
|
19 |
4(66,7%) |
2(33,3%) |
- |
- |
- |
6 |
|
20 |
11(84,6%) |
2(15,4%) |
- |
- |
- |
13 |
|
21 |
7(77,8%) |
2(22,2%) |
- |
- |
- |
9 |
|
Gender | ||||||
|
Male |
27(64,3%) |
12(28,6%) |
3(7,1%) |
- |
- |
42 |
|
Female |
40(69%) |
14(24,1%) |
1(1,7%) |
2(3,4%) |
1(1,7%) |
58 |
|
Accomodation | ||||||
|
Family |
46(75,4%) |
15(24,6%) |
- |
- |
- |
61 |
|
Alone |
18(56,3%) |
9(28,1%) |
2(6,3%) |
2(6,3%) |
1(3,1%) |
32 |
|
Friends |
4(57,1%) |
2(28,6%) |
1(14,3) |
- |
- |
7 |
|
Personality | ||||||
|
Introvert |
21(61,8%) |
8(23,5%) |
2(5,9%) |
2(5,9%) |
1(2,9%) |
34 |
|
Extrovert |
47(71,2%) |
18(27,3%) |
1(1,5%) |
- |
- |
66 |
|
Hobbies | ||||||
|
Hang out with friends |
35(77,8%) |
10(22,2%) |
- |
- |
- |
45 |
|
Play sports |
24(82,8%) |
5(17,2%) |
- |
- |
- |
29 |
|
Read |
5(50%) |
3(30%) |
1(10%) |
1(10%) |
- |
10 |
|
Being alone |
9(56,3%) |
3(18,8%) |
2(12,5%) |
1(6,3%) |
1(6,3%) |
16 |
|
Body weight | ||||||
|
Increased |
4(50%) |
4(50%) |
- |
- |
- |
8 |
|
Decreased |
8(36,4%) |
9(40,9%) |
2(9,1%) |
2(9,1%) |
1(4,5%) |
22 |
|
No change |
56(80%) |
13(18,6%) |
1(1,4%) |
- |
- |
70 |
|
Sleeping difficulty | ||||||
|
Early |
45(90%) |
5(10%) |
- |
- |
- |
50 |
|
Late |
19(55,9%) |
13(38,2%) |
1(2,9%) |
1(2,9%) |
- |
34 |
|
Unable to sleep |
4(25%) |
8(50%) |
2(12,5%) |
1(6,3%) |
1(6,3%) |
16 |
respectively (Table 2).
depression was reporterd by 2(5,9%) students with introverted personality, and by 1(1,5%) student with extroverted personality.
Moderate and severe depression was reported by 2(5,9%) and 1(2,9%) of students with introverted personality (Table 2).
Borderline clinical depression was reported by 1(10%) of students who prefer reading as their hobby, and 2(12,5%) who prefer being alone. Moderate depression was reported by 1 (10%) of those who prefer reading, and 1(6,3%) of those who prefer being alone. Severe depression was reported by 1(6,3%) of students who prefer being alone (Table 2).
Of 22 students with decreased body weight, 2(9,1%) was categorized as borderline depression, 2(9,1%) as moderate depression, and 1(4,5%) as severe depression. Moderate depression was reported by 1(1,4%) of students who reported no change in body weight (Table 2).
Of 34 students reported sleeping late, borderline clinical depression and moderate depression was reported by 1(2,9%) student, respectively. Of 16 students reported unable to sleep, borderline clinical depression was reported by 2(12,5%) students, while moderate and severe
DISCUSSION
Based on BDI scores, 68% of samples was categorized as normal, 26% as mild mood disturbances, 3% as borderline clinical depression, 2% as moderate depression, and 1% as severe depression. Depression was more common in younger students aged 16-17 years old. Based on studies carried out regarding the relationship between age and depression, it is shown that depression is represented by a U-shape graph which means that there is a higher prevalence in the younger age group and older age group.5
Depression was more common in female compared to male students. Furthermore, moderate and severe depression was reported only in female students. Based on a universal observation, there is a prevalence of two times higher of depression disorder in women than in men regardless of their country or culture.6 Studies also shown that based on gender differences there is a higher possibility of females to undergo depression as compared to males. However
3
the findings differ based on the onset, duration and episode of depression. It is also reported that females face a higher risk of depression at earlier age than may have a predominant factor to adult depression.7
Based on accomodation, depression was more common in students living alone compared to those living with family or friends. During university life, it is common for students to live in a shared rental accommodation, which may benefit in terms of reduced costs and increase moral/ social support. However, being far from home and away from family can be a cause of depression among students. Being alone is also another cause of depression.8
Based on personality trait, depression was more common in those with introverted personality, and regarding hobbies, depression was more common in students who prefer reading and being alone. However, studies shown that no single personality trait or type uniquely predisposes a person to depression; all humans, of
whatever personality pattern, can and do become depressed under appropriate circumstances. Persons with certain personality disorders-OCD, histrionic, and borderline may be at greater risk for depression than persons with antisocial or paranoid personality disorder.6
Depression was more common in students reporting decreased body weight. This probably caused by decreased appetite (anhedonia) which is one of the hallmark of depression. Studies shown that many depressive patients have decreased appetite and weight loss, but others may experience increased appetite and weight gain and sleep longer than usual.6
Depression was also more common in students who sleeps late and those reporting unable to sleep. Studies shown that students whose sleep duration is less than 6 hours and those whose sleep duration is more than 8 hours are tended to be more depressed than those whose sleep duration is between 6 to 8 hours. A study shows that sleep duration exhibited a U-shaped association with symptoms of depression. As subjective sleep sufficiency decreased, symptoms of depression increased, indicating a linear inverse-proportional relationship.9
CONCLUSION
Of 100 samples, 68% was categorized as normal, 26% as mild mood disturbances, 3% as borderline clinical depression, 2% as moderate
depression, and 1% as severe depression. Depression was more common in younger students aged 16-17 years old, female, students who lives alone, those with introverted personality, students who prefer reading and being alone, and those reported decreased body weight and sleeping difficulty.
REFERENCES
-
1. Marcus M, Yasamy MT, Ommeren Mv, Chisholm D, Sax S. Depression: A Global Public Health Concern Geneva: WHO Department of Mental Health and Substance Abuse; 2012.
-
2. Kumaraswamy N. Academic Stress, Anxiety and Depression among College Students- A Brief Review. International Review of Social Sciences and Humanities. 2013; 5(1): p. 135-143.
-
3. Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a crosssectional study. Medical Education. 2005; 39(6): p. 594-604.
-
4. Rosal M, Ockene I, Ockene J, Barrett S, Ma Y, Hebert J. A longitudinal study of students' depression at one medical school. Academic Medicine. 1997; 72(6): p. 524-526.
-
5. Tomitaka S, Kawasaki Y, Ide K, Yamada H, Furukawa T, Ono Y. Age-related changes in the distributions of depressive symptom items in the general population: a cross-sectional study using the exponential distribution model. PeerJ. 2016; 5(4): p. e1457.
-
6. Saddock BK, Saddock VA, Ruiz P. Mood Disorders. In Kaplan & Saddock's Synopsis of Psychiatry. New York: Lippinscott Willlims & Wilkins; 2007. p. 527-576.
-
7. Piccinelli M, Wilkinson G. Gender differences in depression: Critical review. The British Journal of Psychiatry. 2000; 177(6): p. 486-492.
-
8. Khawaja N, Duncanson K. Using the University Student Depression Inventory to Investigate the Effect of Demographic Variables on Students' Depression. Australian Journal of Guidance and Counselling. 2008; 18(2): p. 195-209.
-
9. Kaneita Y, Ohida T, Uchiyama M, Takemura S, Kawahara K, Yokoyama E, et al. The Relationship Between Depression and Sleep Disturbances. The Journal of Clinical Psychiatry. 2006; 67(2): p. 196-203.
Discussion and feedback